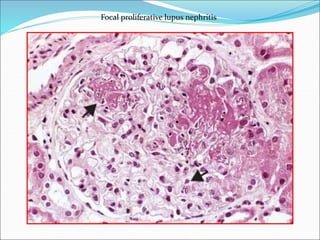
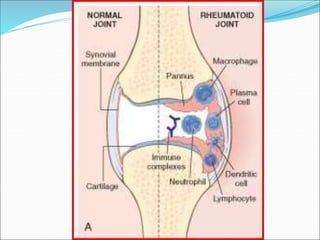
The document discusses several autoimmune diseases including systemic lupus erythematosus, rheumatoid arthritis, Sjögren's syndrome, systemic sclerosis, and mixed connective tissue disease. It provides details on the pathogenesis, clinical features, immunological characteristics, and morphology of these conditions. Autoimmune diseases result from a loss of tolerance to self-antigens and can involve deregulated immune responses against tissues and organs, leading to inflammation and damage.