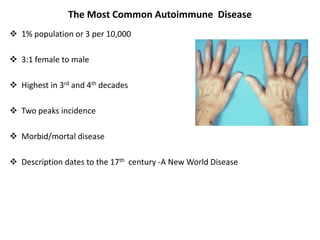
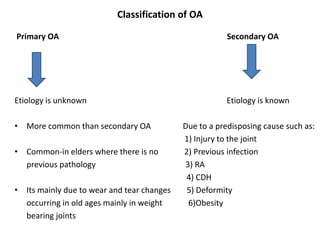
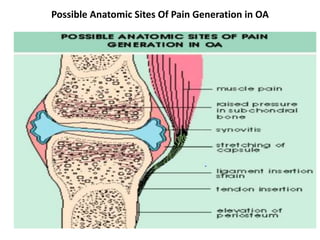
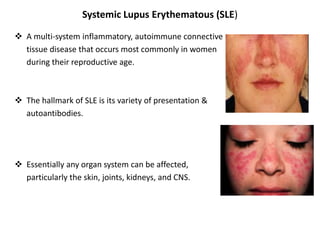
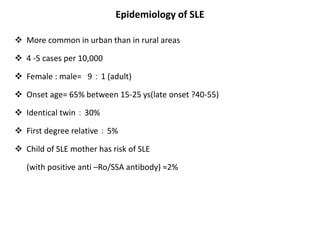
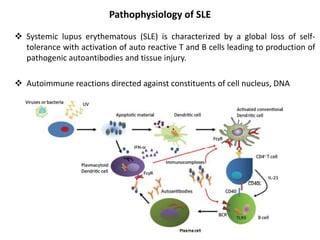
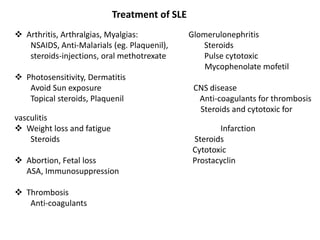
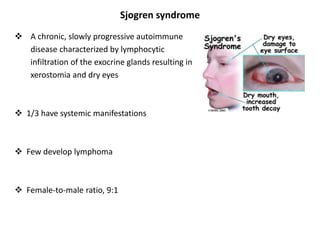
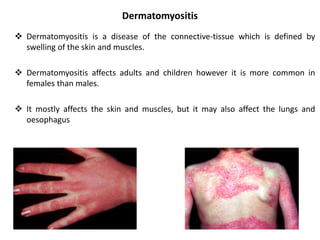
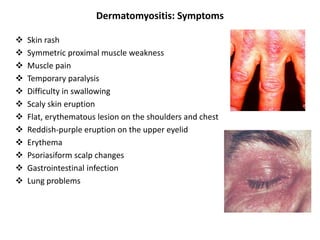
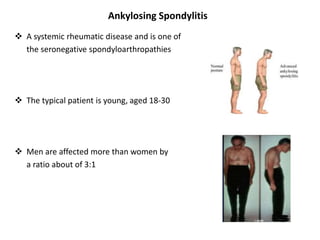
Rheumatological diseases can affect the joints, skin, and internal organs. Some common types include rheumatoid arthritis, osteoarthritis, lupus, Sjogren's syndrome, and spondyloarthropathies like ankylosing spondylitis. Rheumatoid arthritis causes chronic inflammation of the synovium and can lead to joint deformity. Osteoarthritis is characterized by cartilage loss within a joint and associated bone changes. Systemic lupus erythematosus is a multi-system autoimmune disease affecting many organs, with a variety of potential manifestations.