This document provides an overview of atrial fibrillation (AF), including statistics on prevalence, pathophysiology, types, treatment goals, and medication options. Some key points:
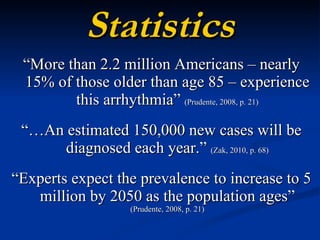
- AF affects over 2 million Americans and is expected to increase to 5 million by 2050 due to an aging population.
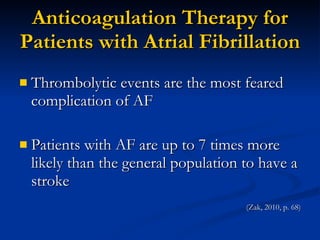
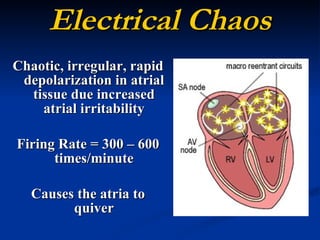
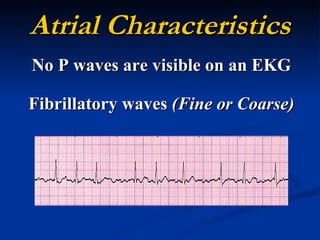
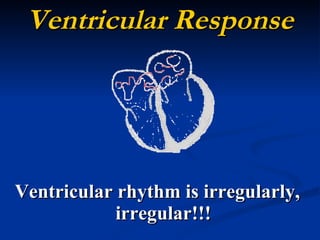
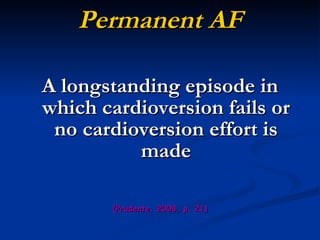
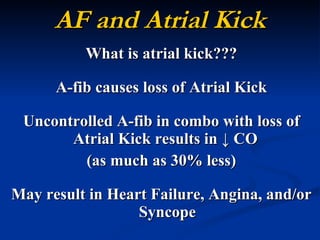
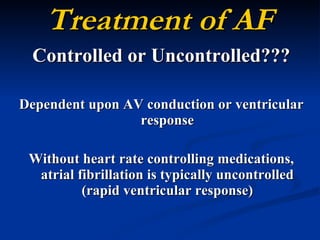
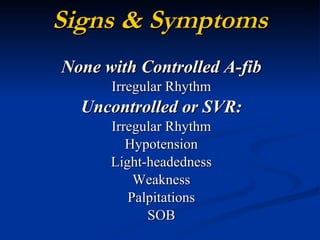
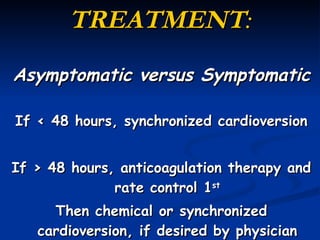
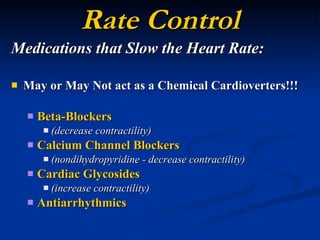
- It involves chaotic electrical activity in the atria causing irregular heartbeat. Treatment aims to restore normal rhythm or control heart rate while preventing clots.
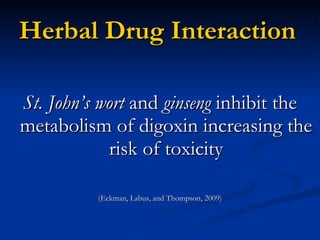
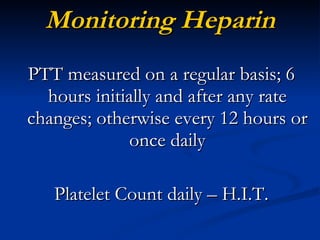
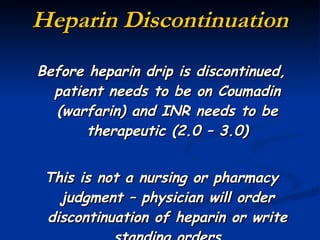
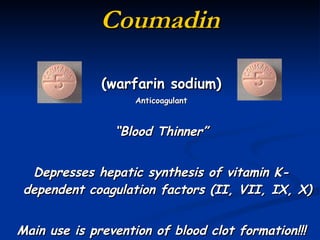
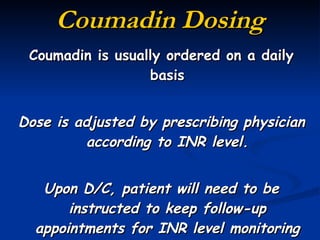
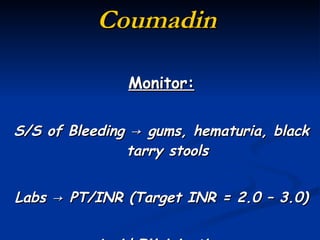
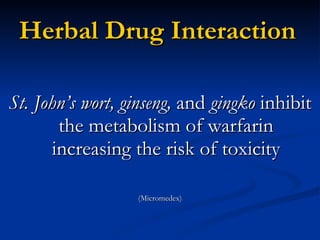
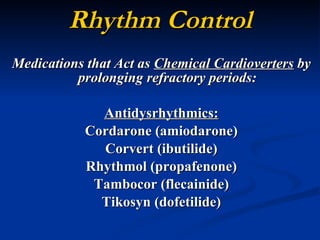
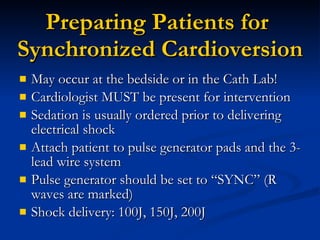
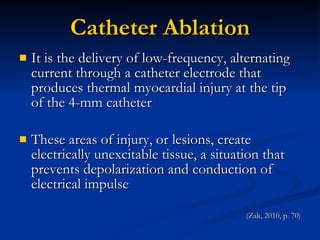
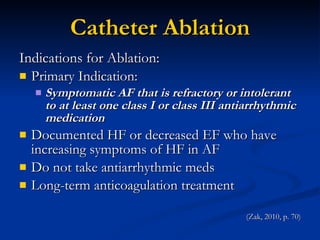
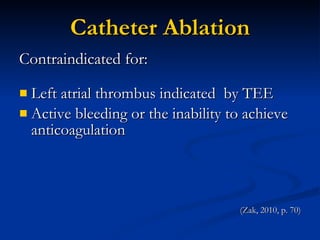
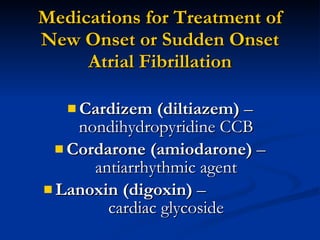
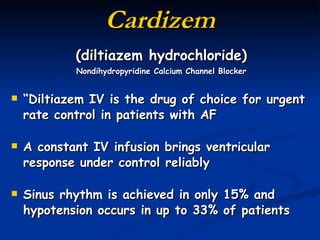
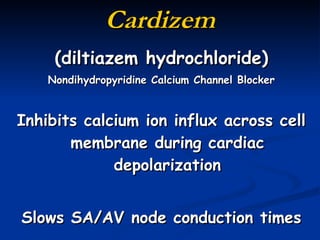
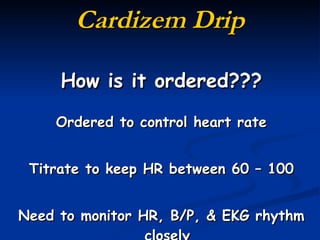
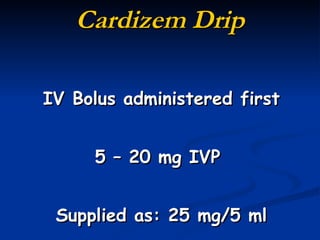
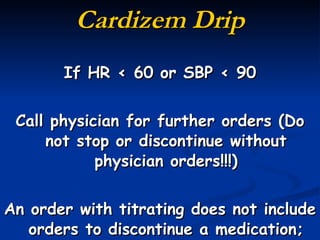
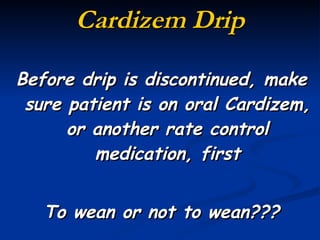
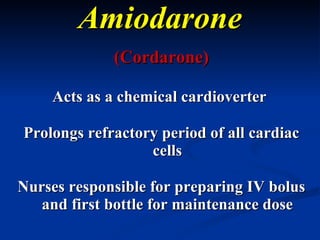
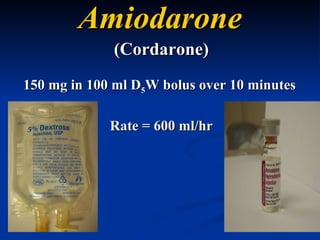
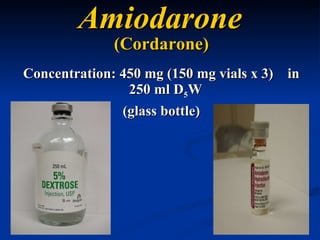
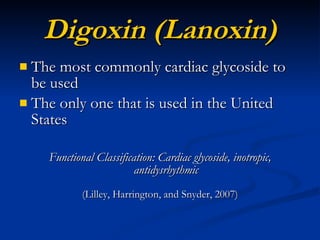
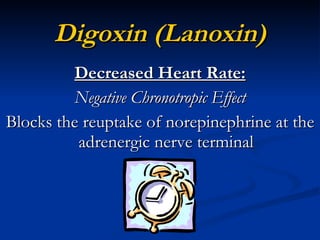
- Options include electrical or chemical cardioversion, catheter ablation, and medications to restore rhythm or slow heart rate such as amiodarone, diltiazem, digoxin, and beta blockers. Anticoagulants like heparin and
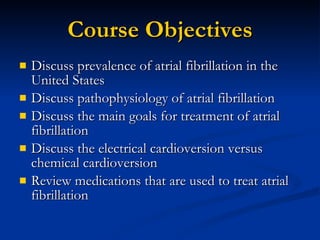











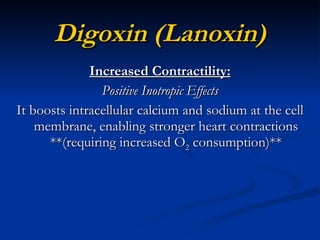


![Adverse Reactions/Side Effects Digoxin Toxicity [has a narrow therapeutic index – (0.5 – 2 ng/ml)] Bradycardia Arrhythmias, complete heart blocks Nausea, vomiting Abdominal pain, diarrhea Headache, vision changes Irritability, insomnia, depression (Eckman, Labus, and Thompson, 2009, p. 184)](https://image.slidesharecdn.com/atrialfibrillation2010-110705132757-phpapp01/85/Atrial-Fibrillation-BMH-Tele-57-320.jpg)