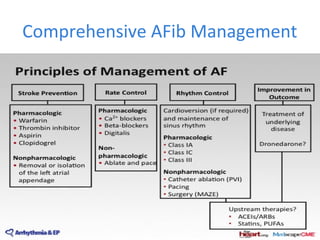
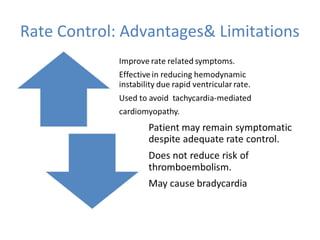
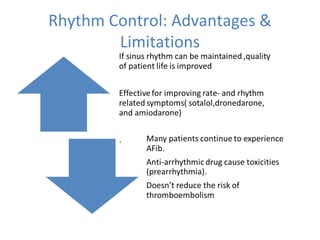
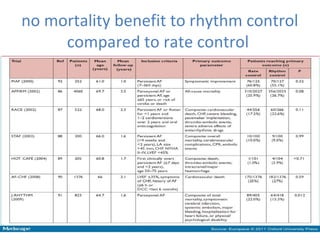
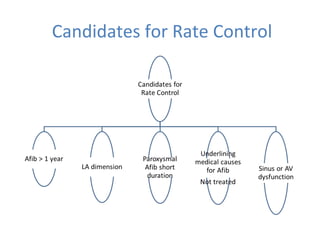
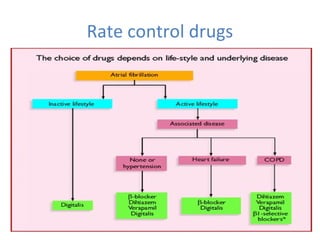
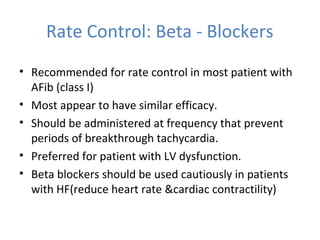
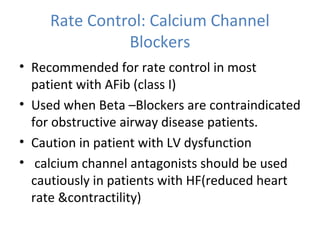
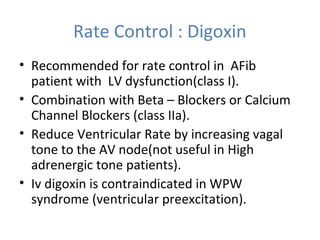
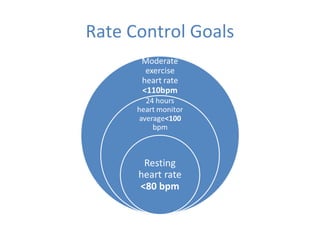
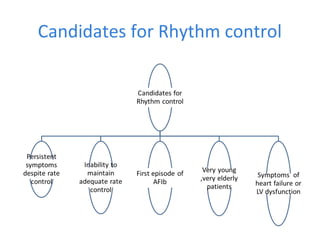
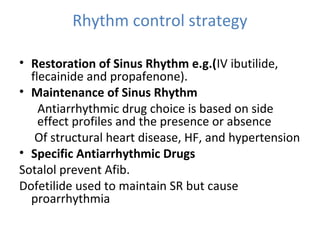
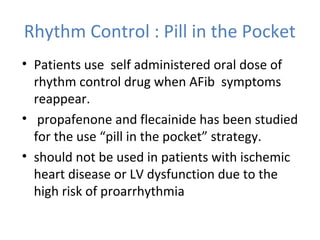
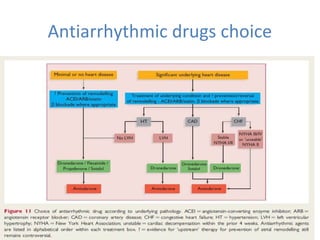
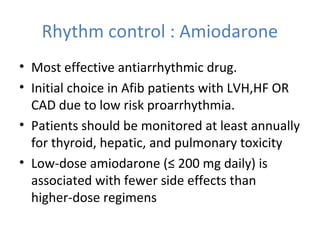
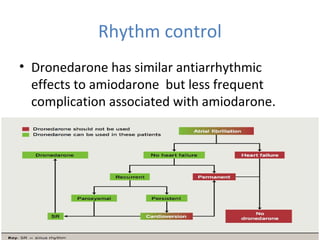
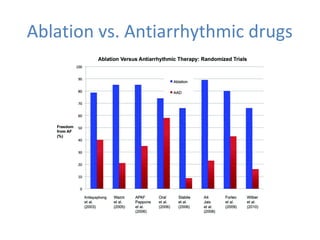
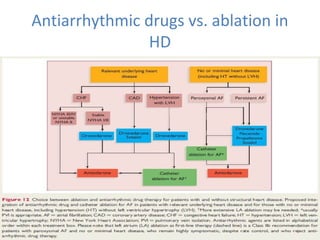
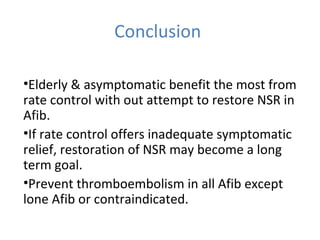
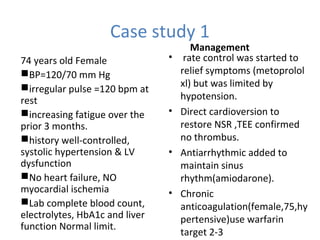
This document summarizes guidelines for rate and rhythm control for atrial fibrillation. It discusses using medications like beta blockers, calcium channel blockers, and digoxin for rate control. For rhythm control, electrical cardioversion or antiarrhythmic drugs may be used to restore normal sinus rhythm, with amiodarone being preferred for patients with heart failure or coronary artery disease due to its lower risk of side effects. The document also discusses when rate control versus rhythm control strategies are preferred based on patient characteristics and presents a case study on managing a patient with atrial fibrillation.