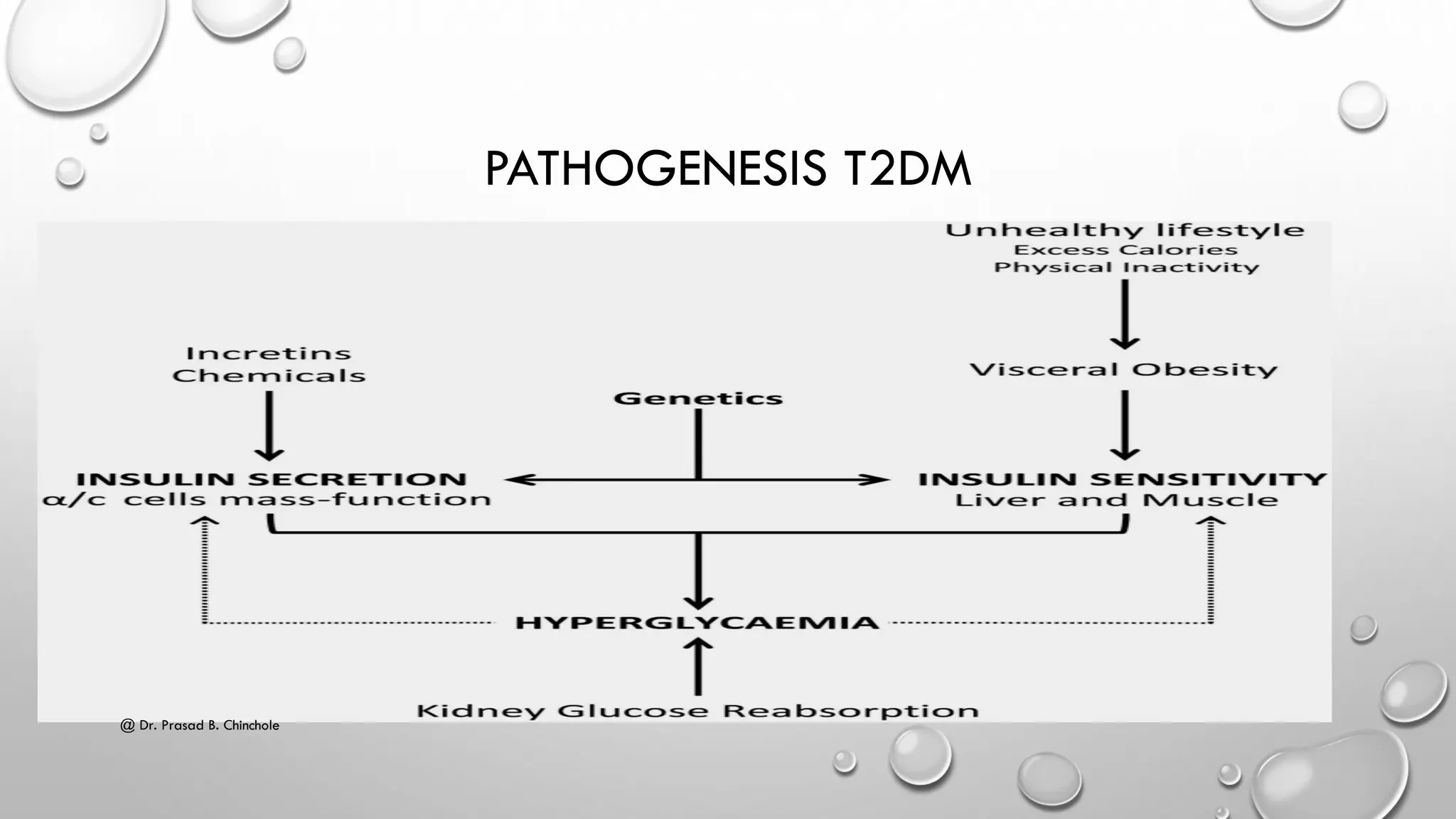
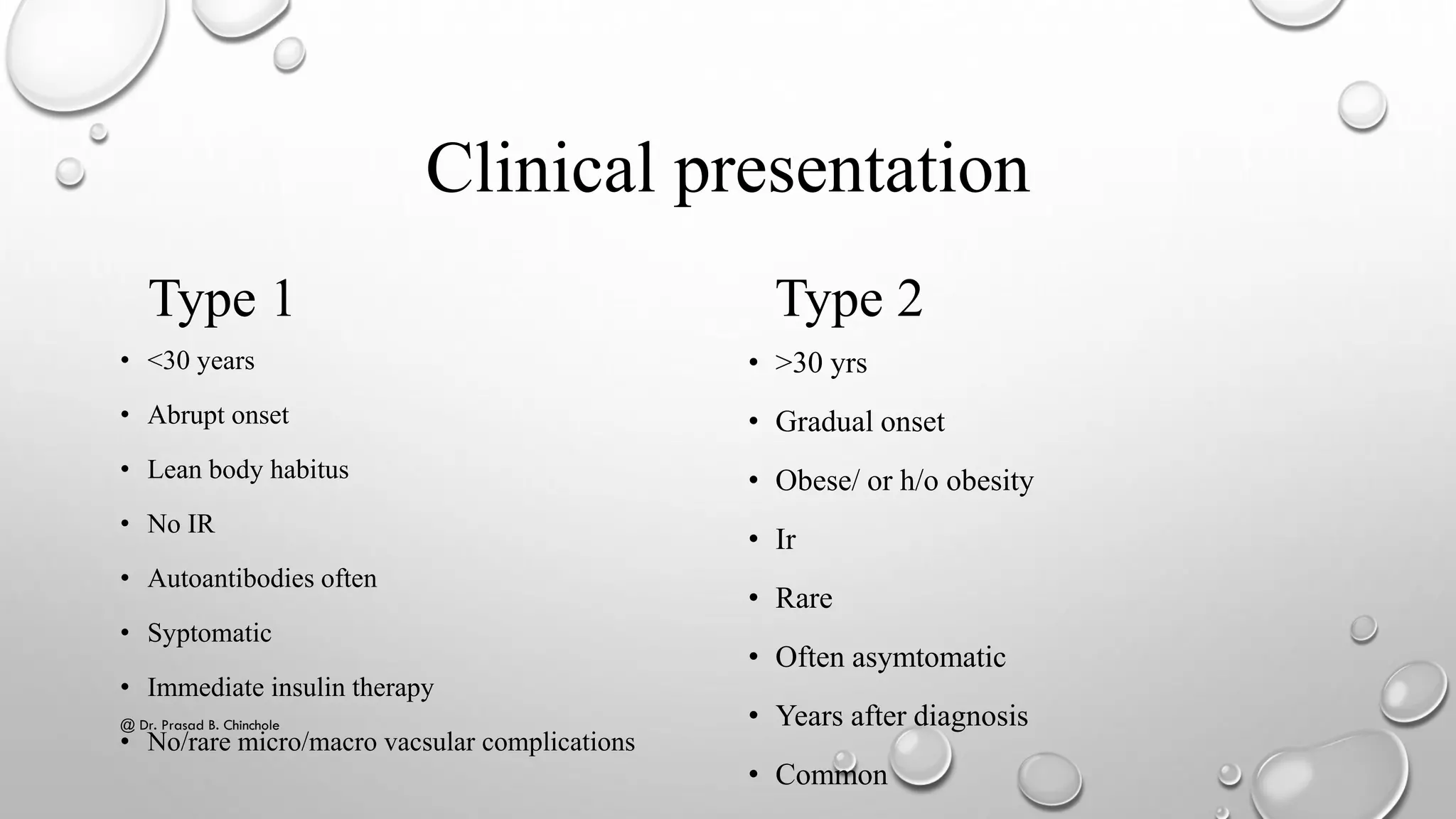
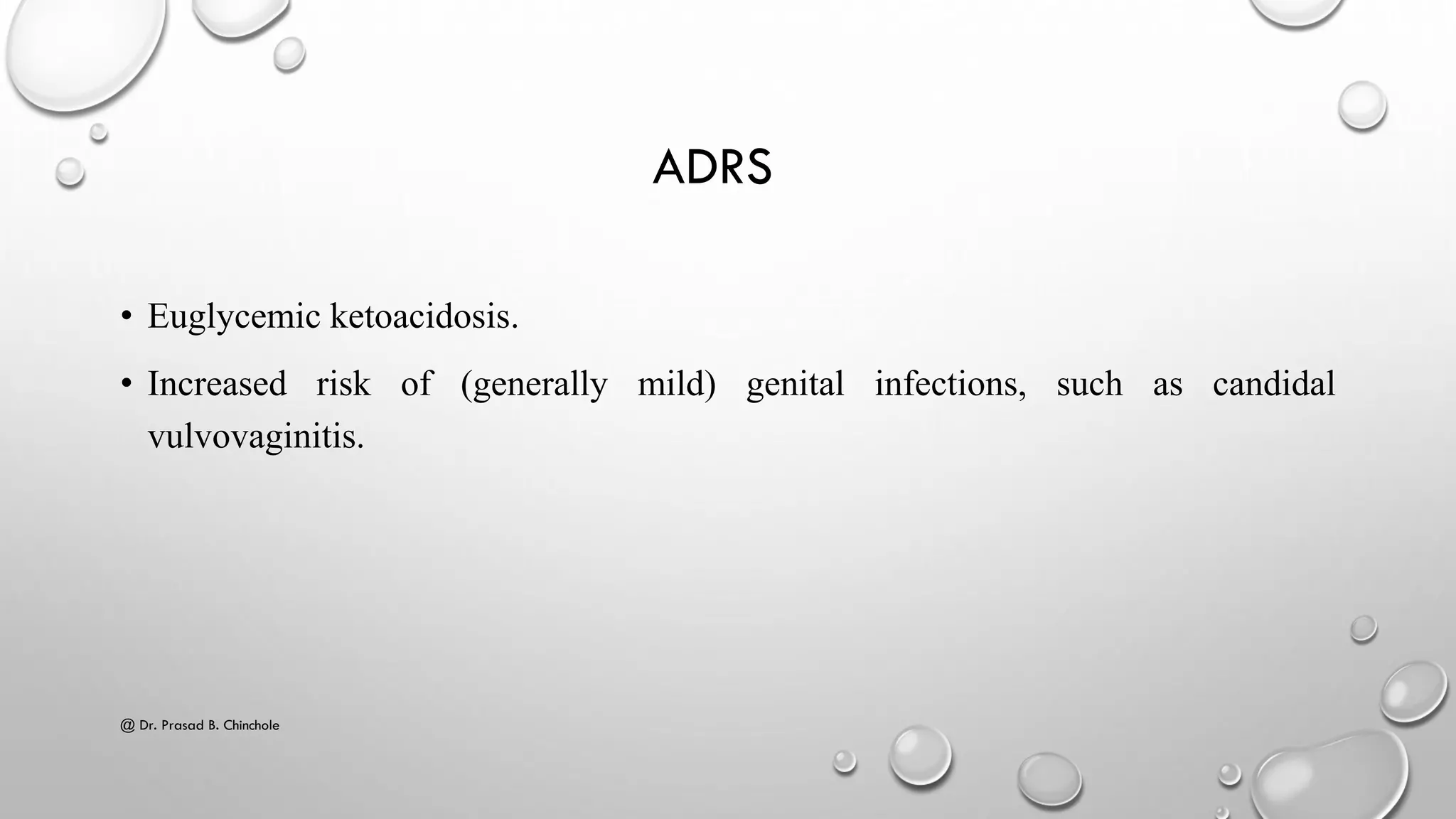
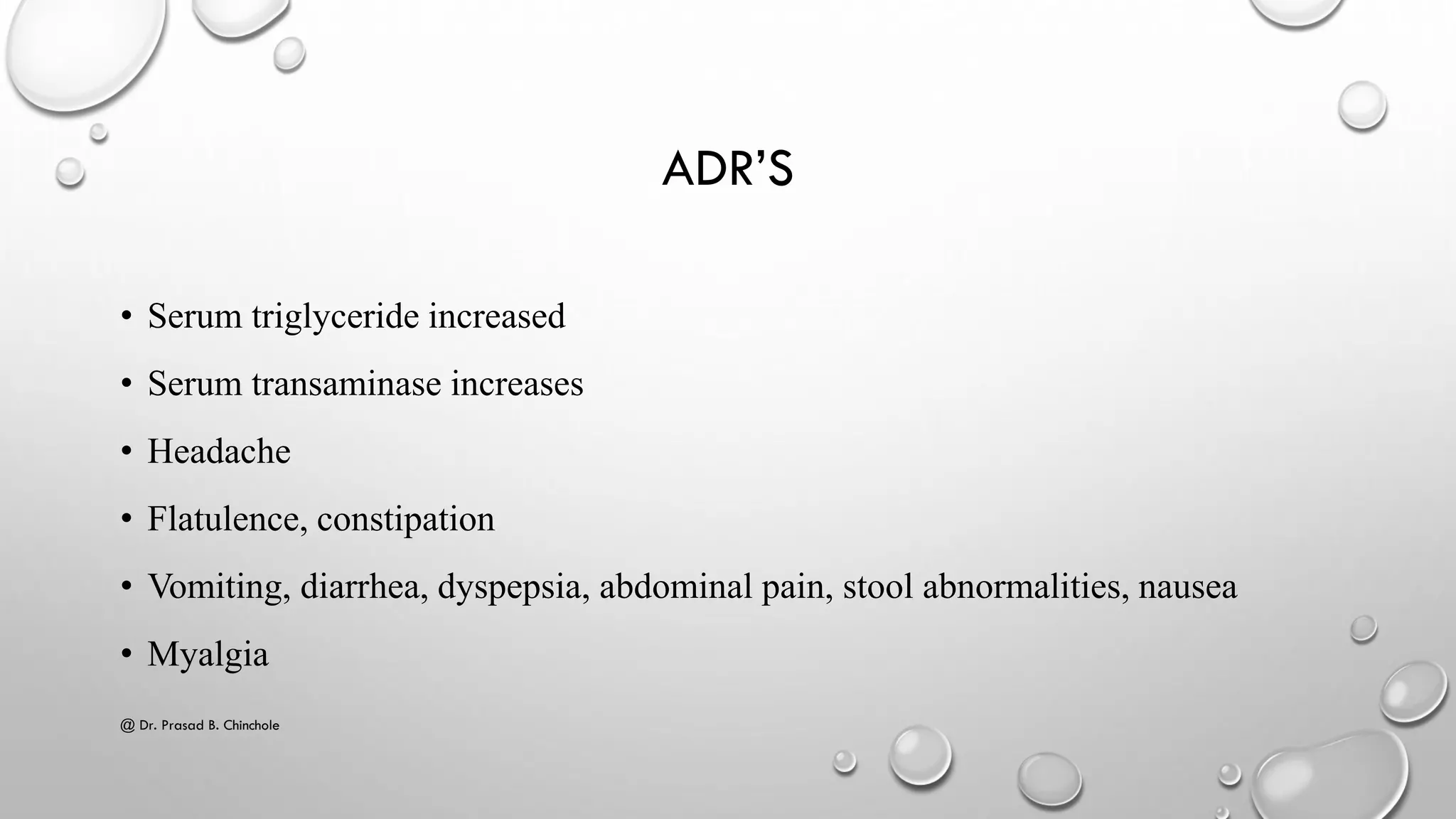
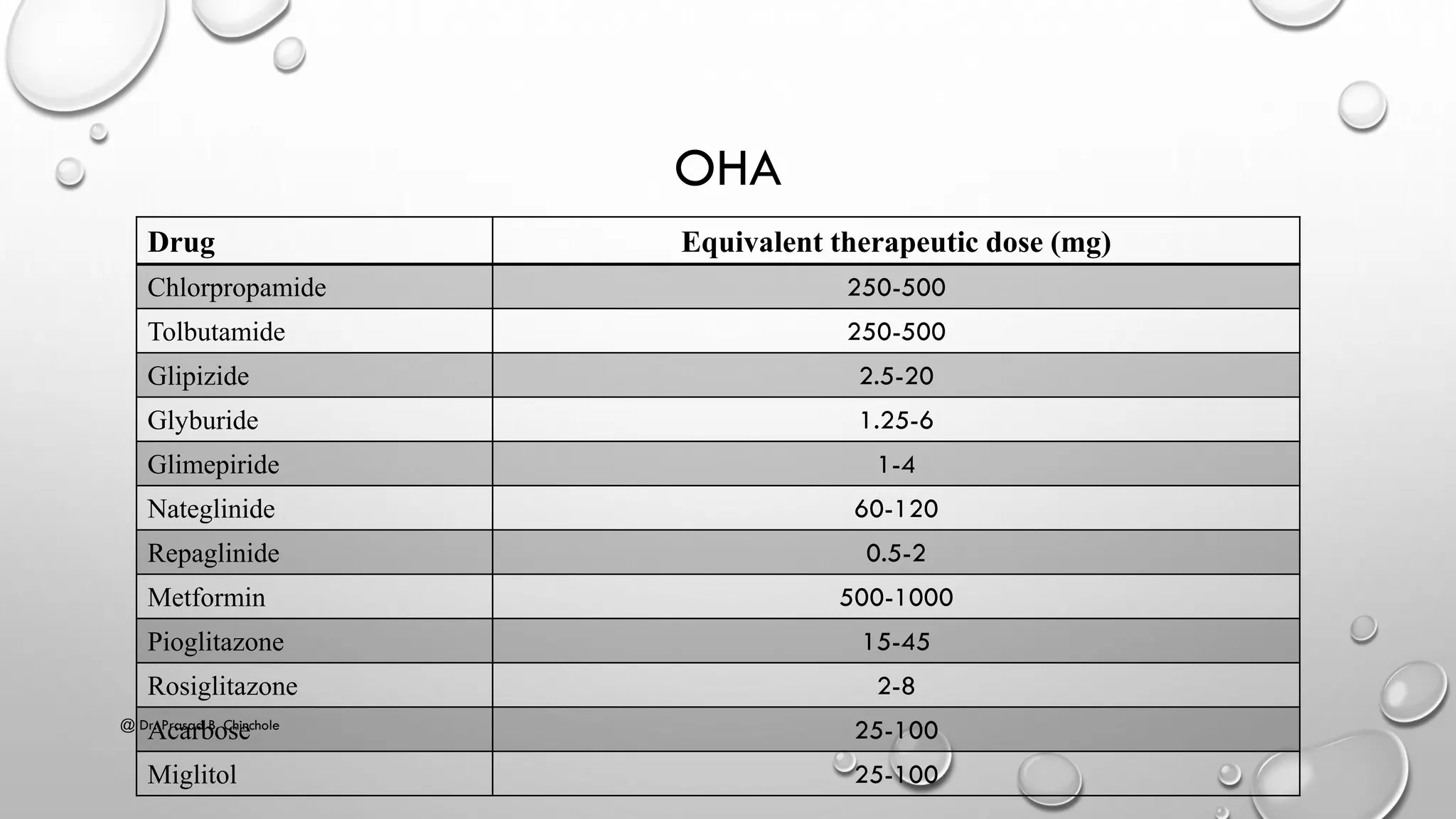
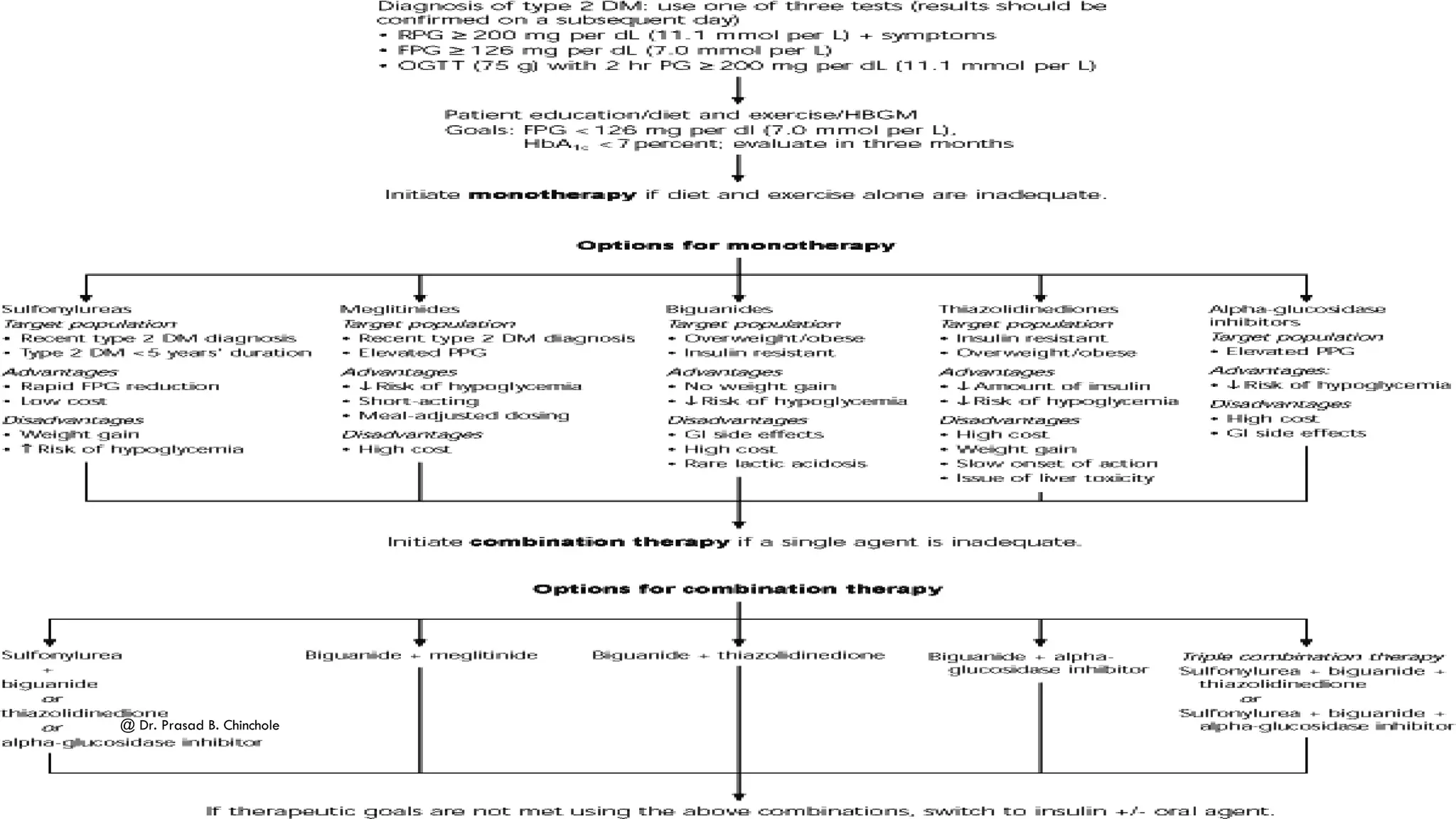
The document provides a comprehensive overview of diabetes mellitus, covering its classification (Type 1, Type 2, gestational diabetes), epidemiology, pathogenesis, diagnosis, and treatment options. It details the differences between Type 1 and Type 2 diabetes, clinical presentation, screening recommendations, and the role of insulin therapy along with non-pharmacological approaches. Additionally, it outlines various medication classes, their mechanisms of action, and potential side effects.