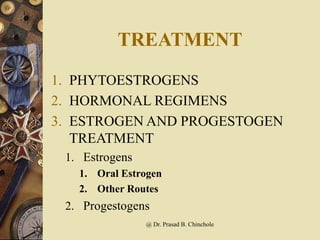
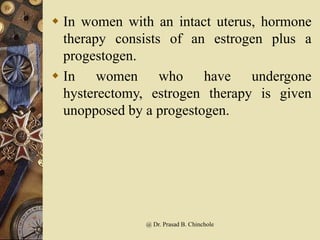
Hormone replacement therapy (HRT) involves supplemental estrogen, progesterone, and sometimes testosterone to treat symptoms of menopause. It can help reduce hot flashes, night sweats, and risks of osteoporosis and heart disease, but also increases risks of blood clots, stroke, and breast cancer. HRT regimens include continuous or intermittent combinations of estrogen and progesterone in pills, patches, or other forms for varying numbers of days per month. The benefits and risks should be considered on an individual basis.