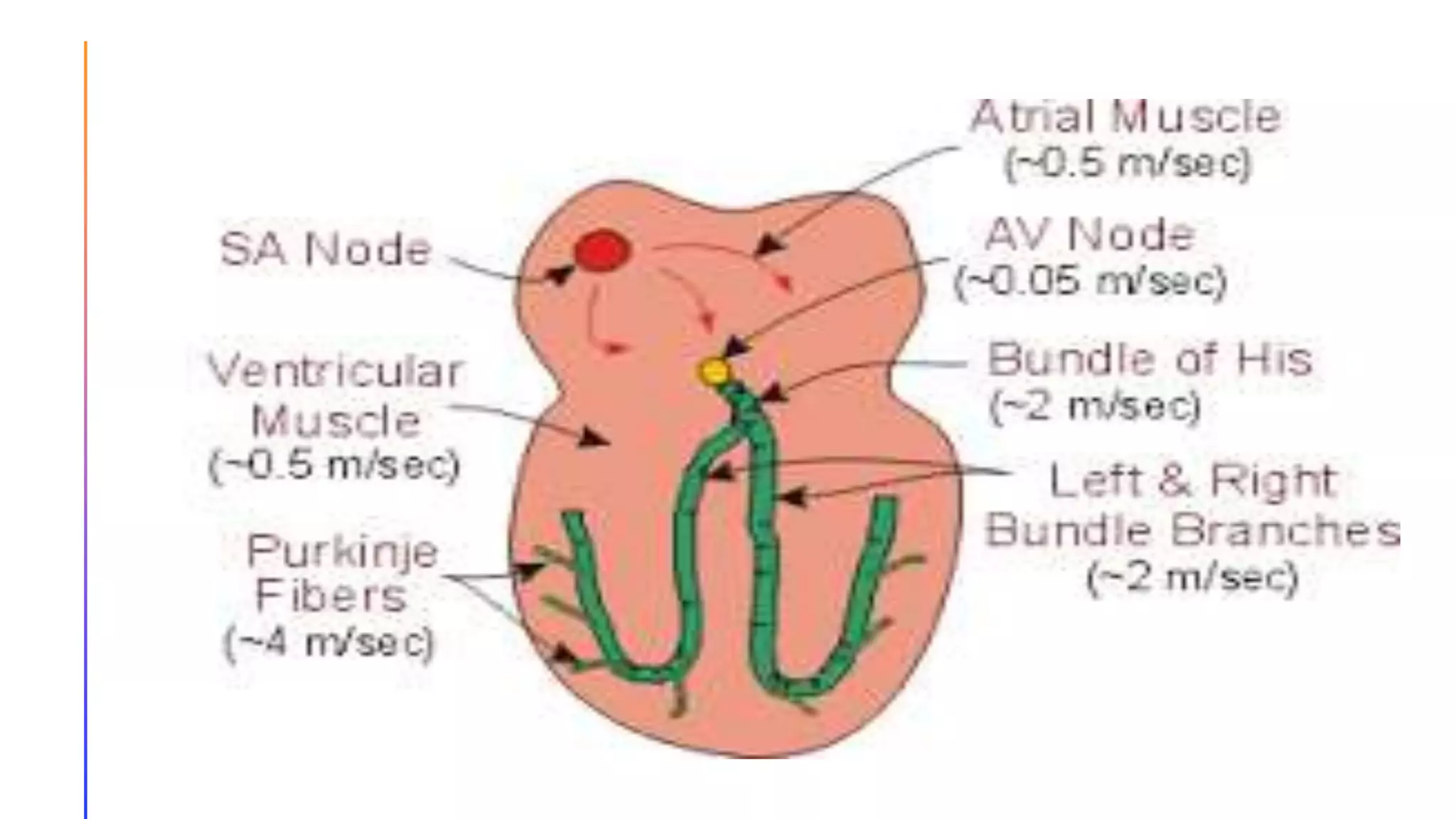
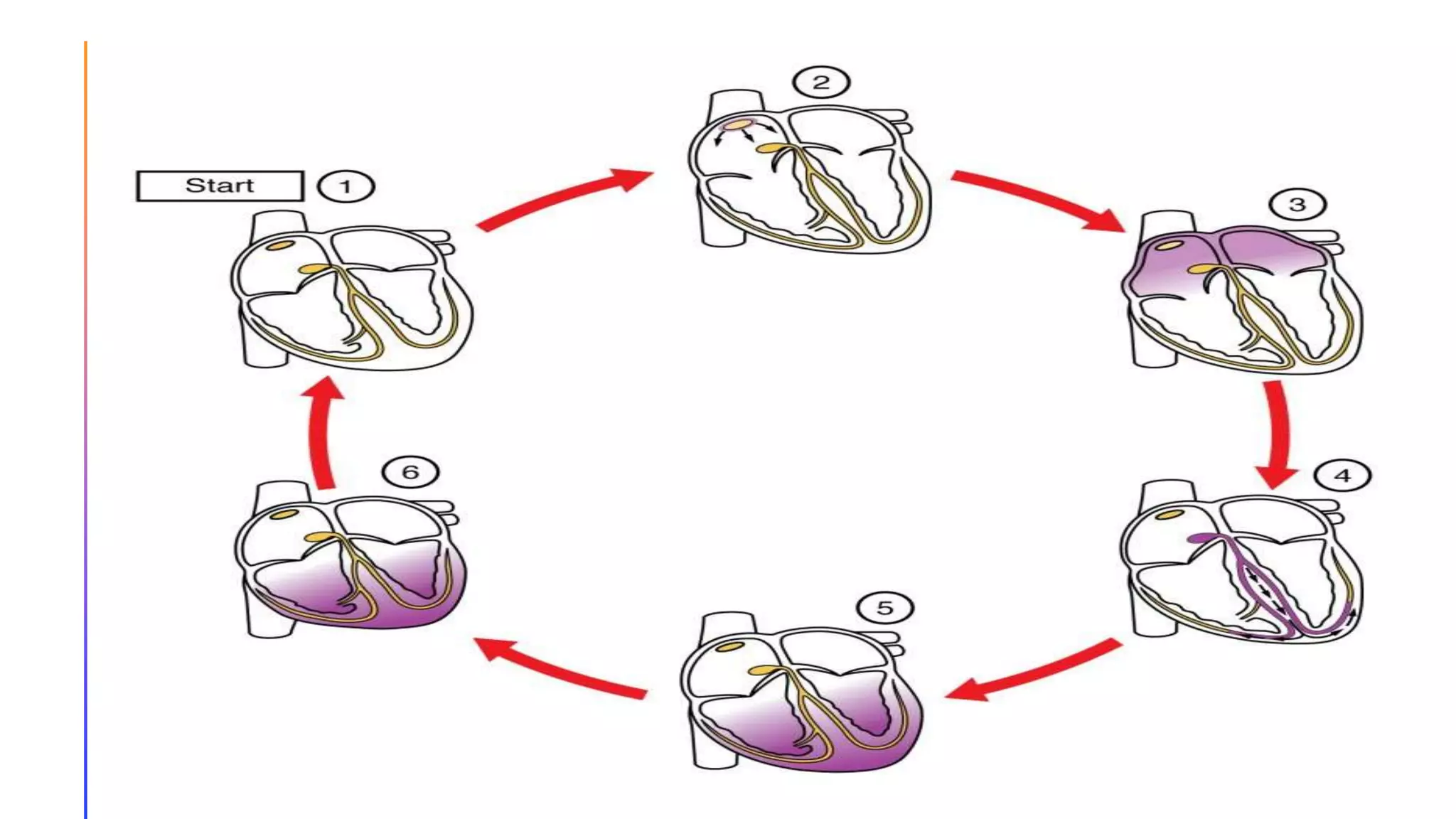
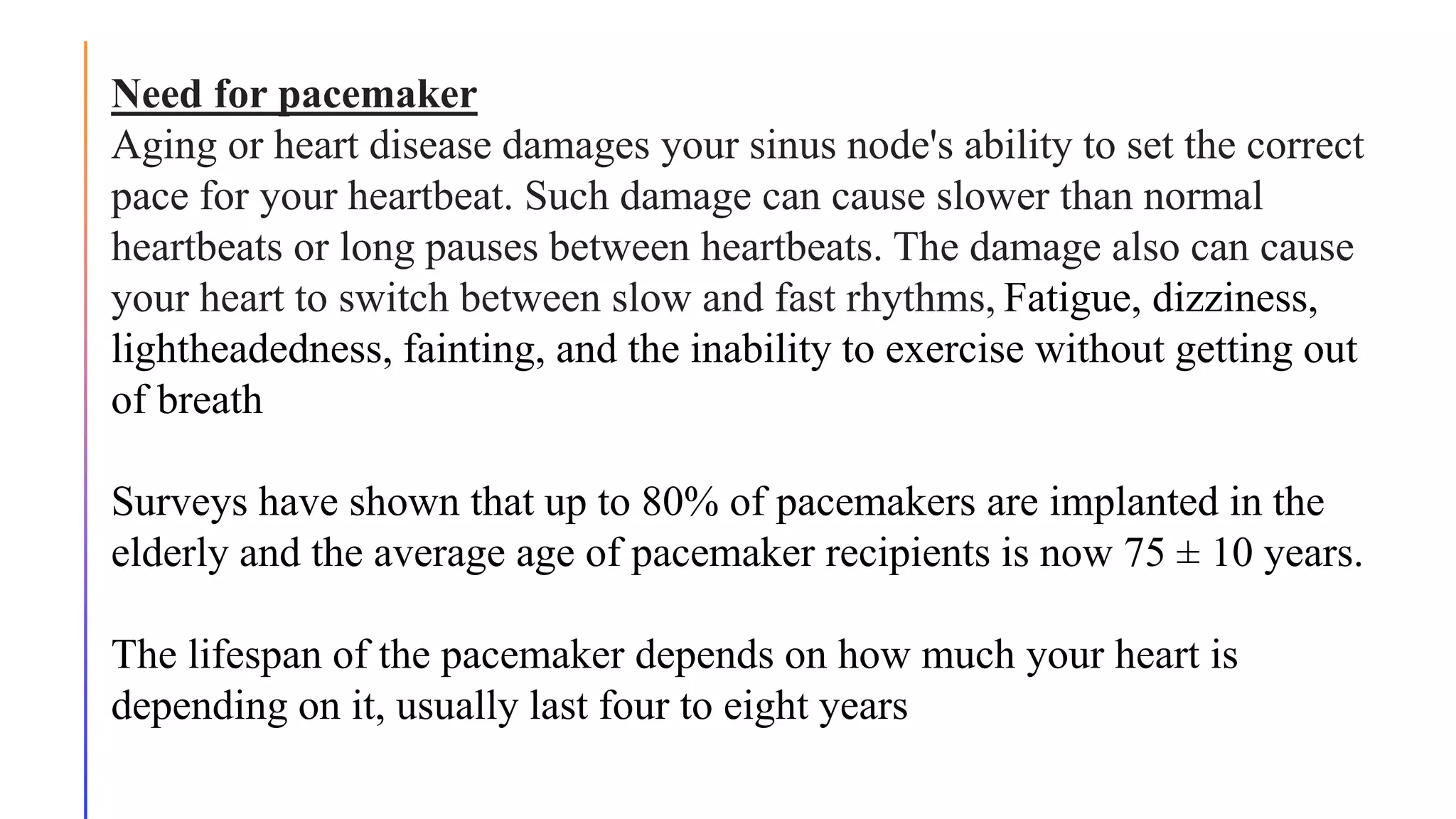
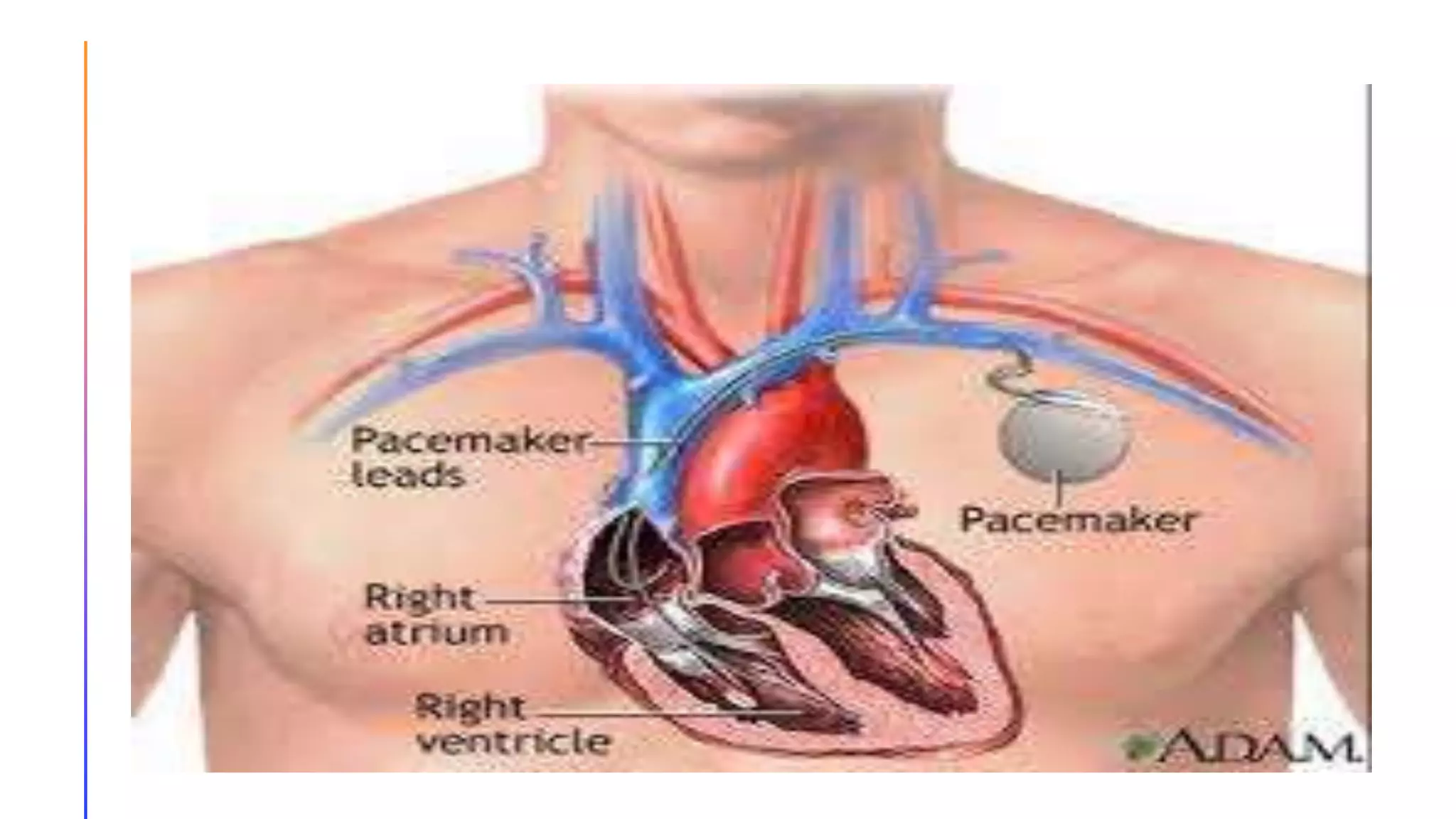
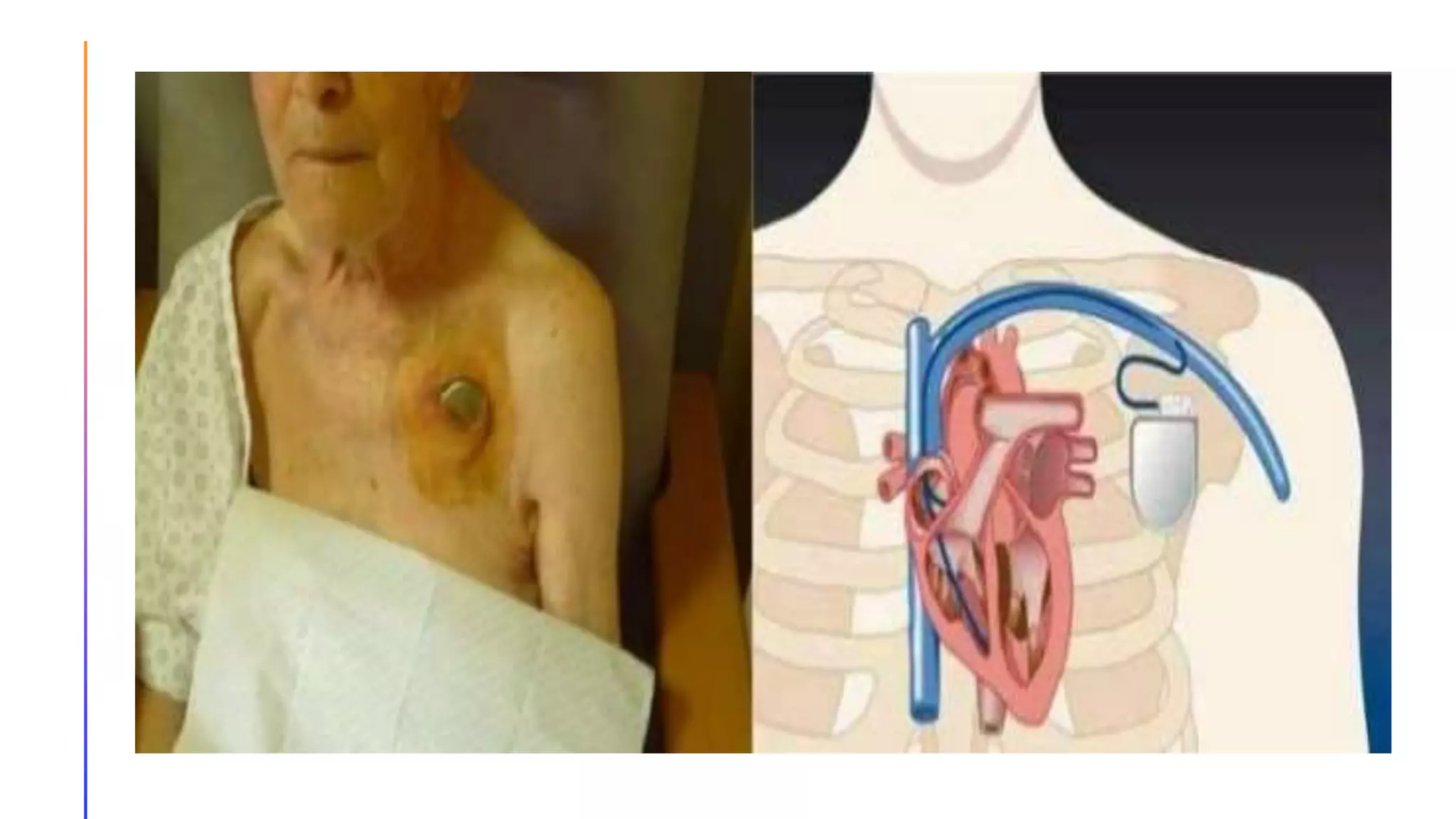
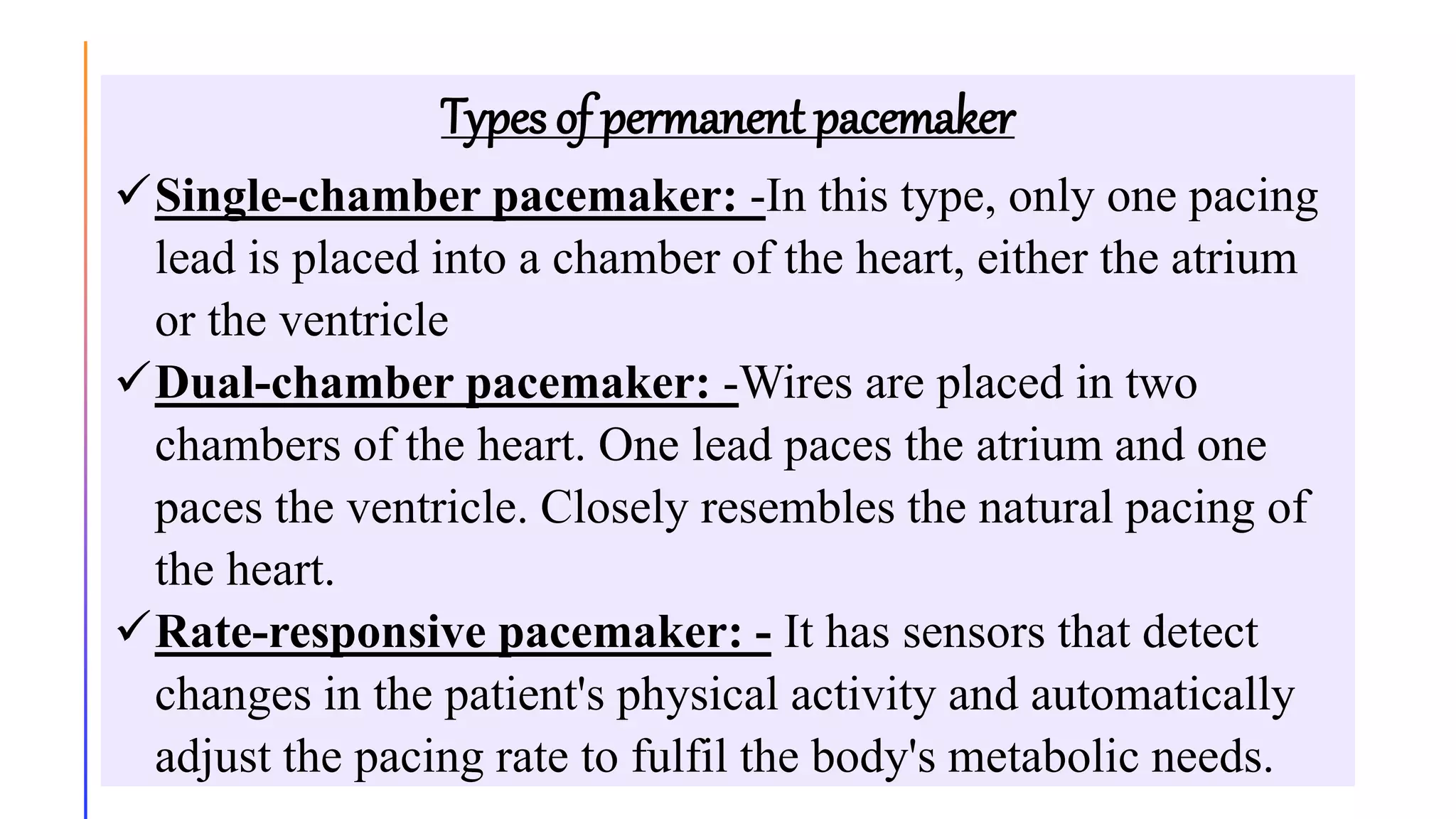
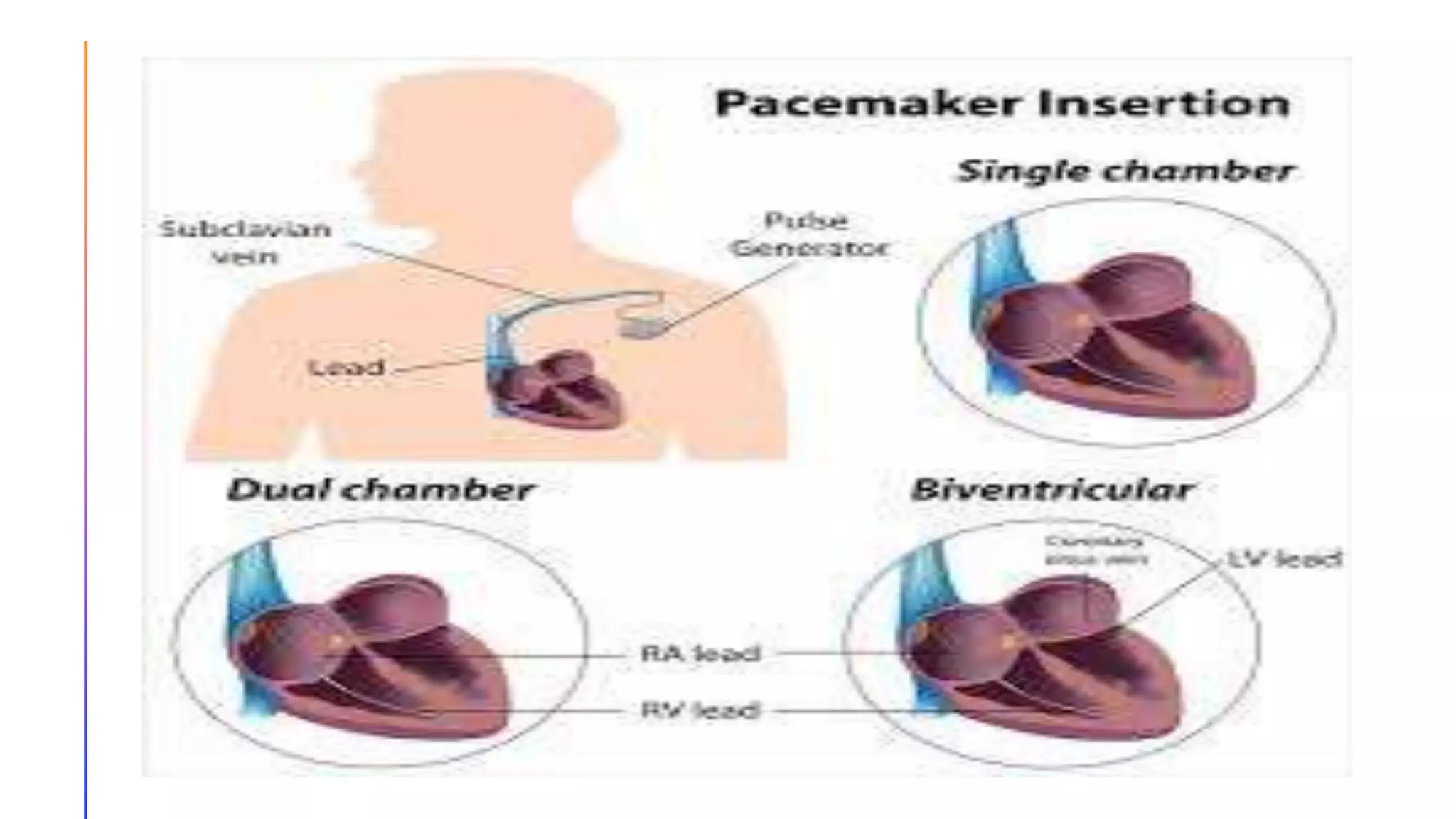
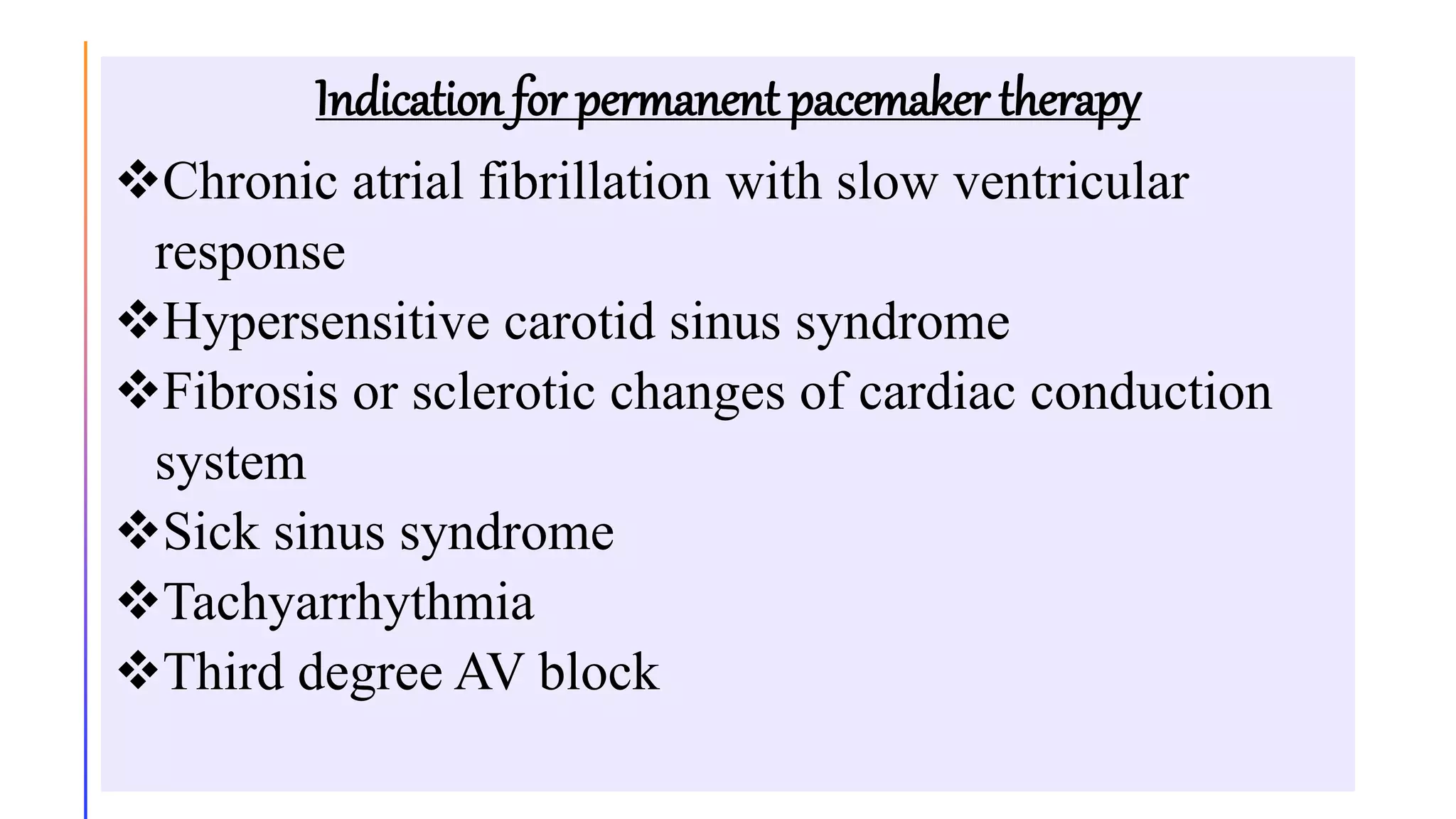
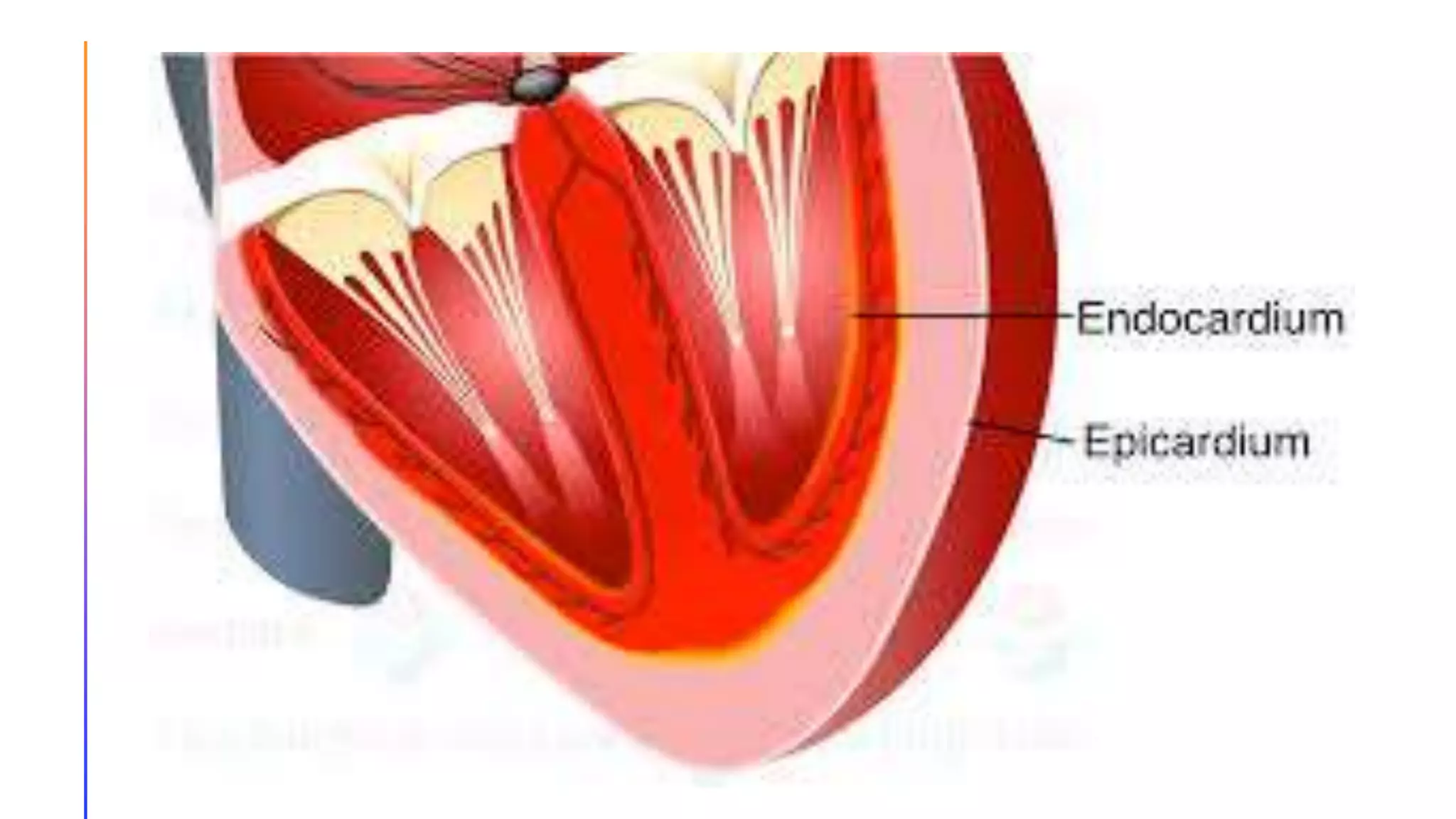
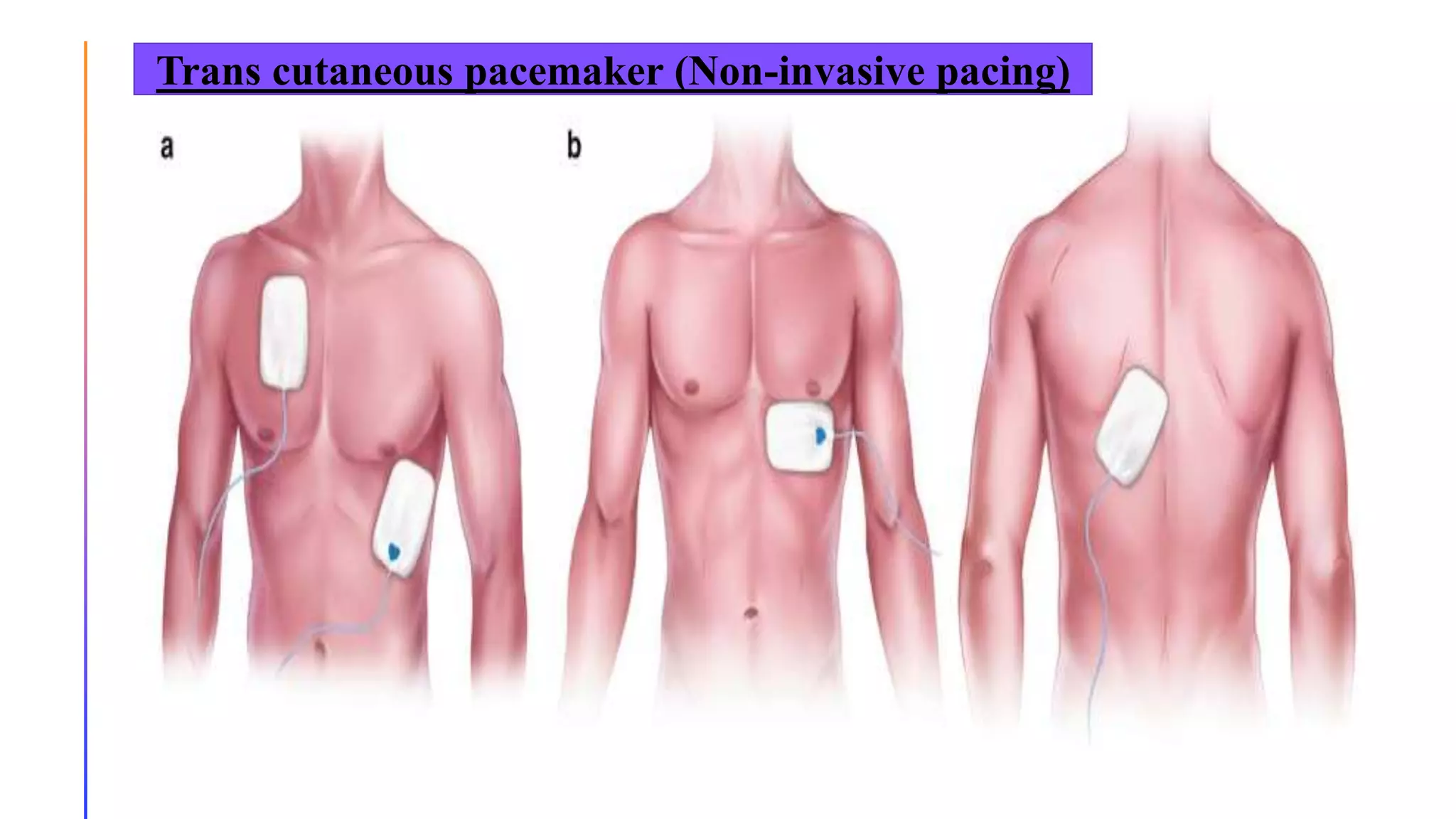
A cardiac pacemaker is an electronic device that regulates heartbeats when the heart's natural system is impaired, typically used in elderly patients with conditions like sick sinus syndrome or chronic atrial fibrillation. Pacemakers consist of a pulse generator and electrodes, which can be either permanent or temporary, with varying types catering to specific needs. Proper nursing management before, during, and after pacemaker implantation is crucial to prevent complications and ensure patient education on care and monitoring.