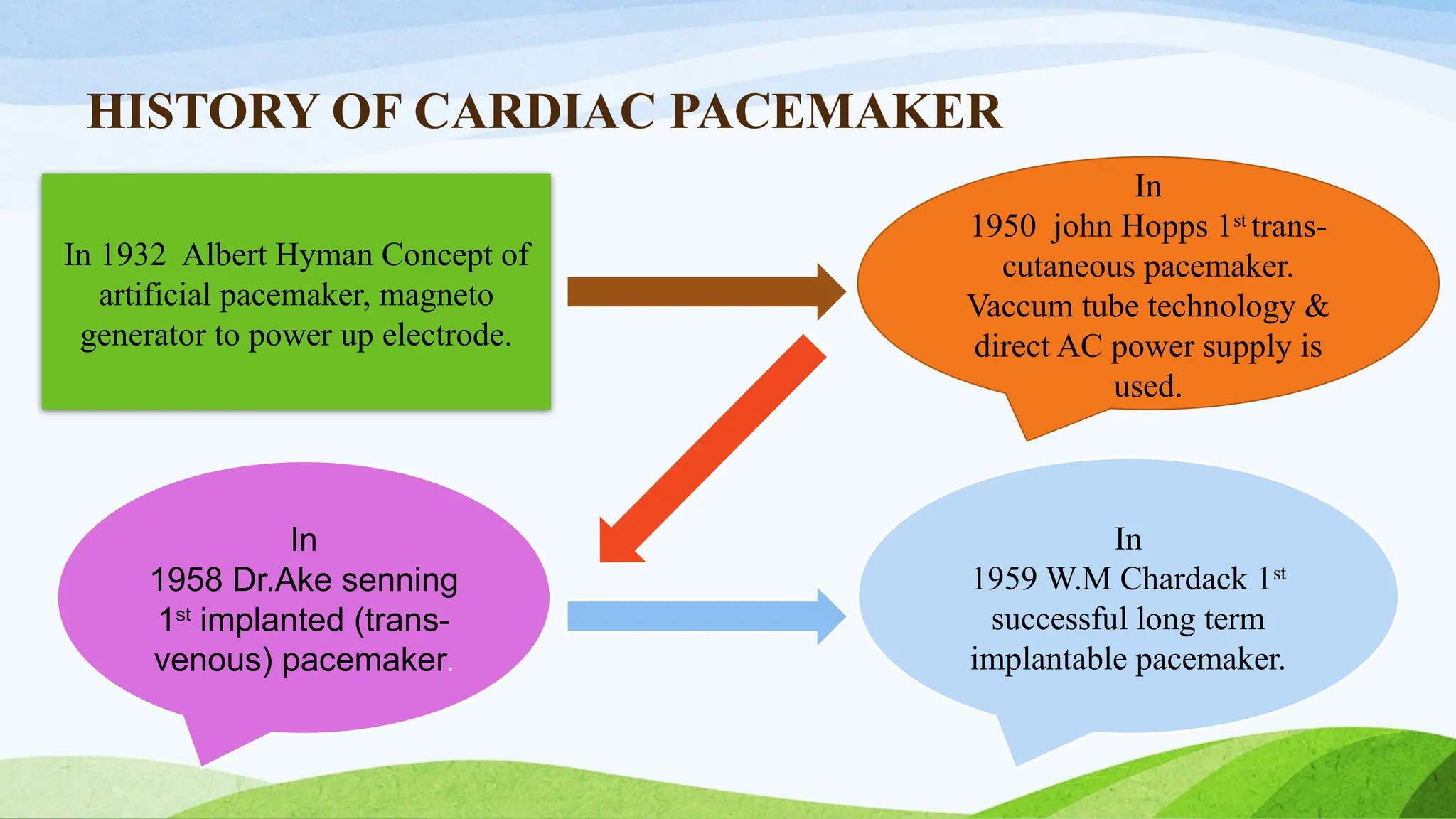
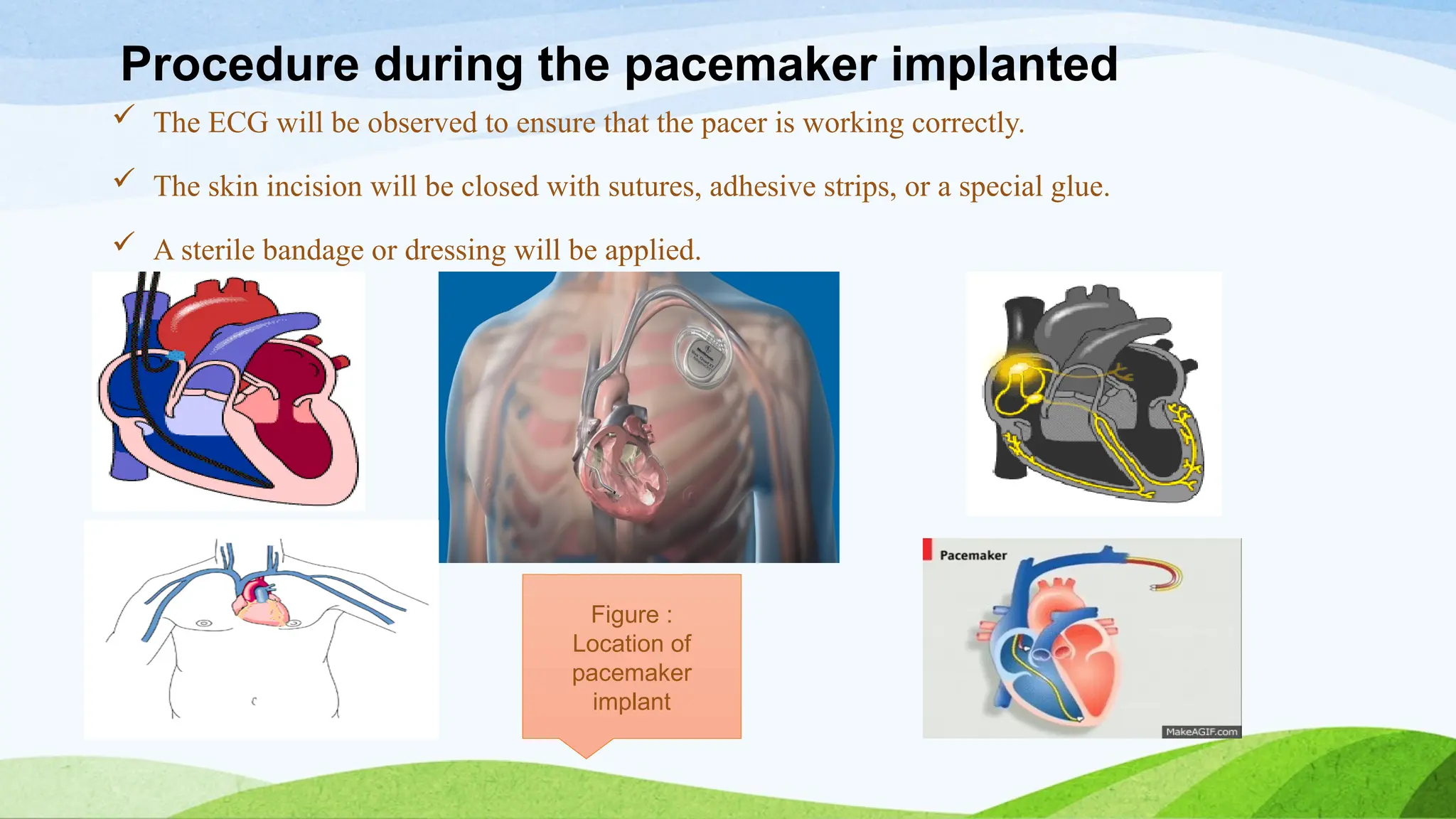
The document provides a comprehensive overview of cardiac pacemakers, describing their function, types, indications, and history. It outlines the purposes of both temporary and permanent pacemakers, detailing the implantation procedures, types of devices, operational modes, and potential malfunctions. It also includes patient management strategies, assessments, and education regarding the care of pacemakers.