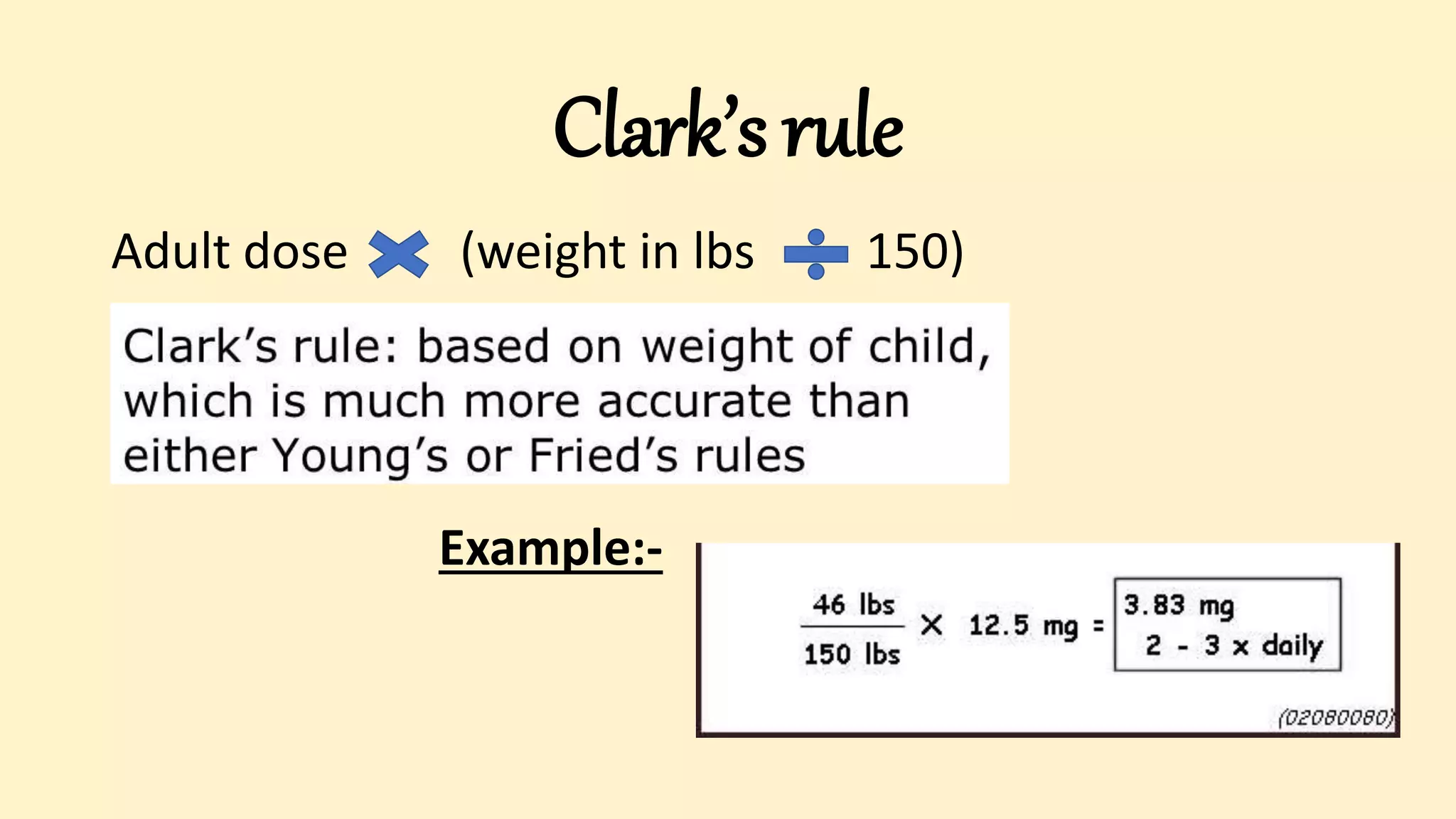
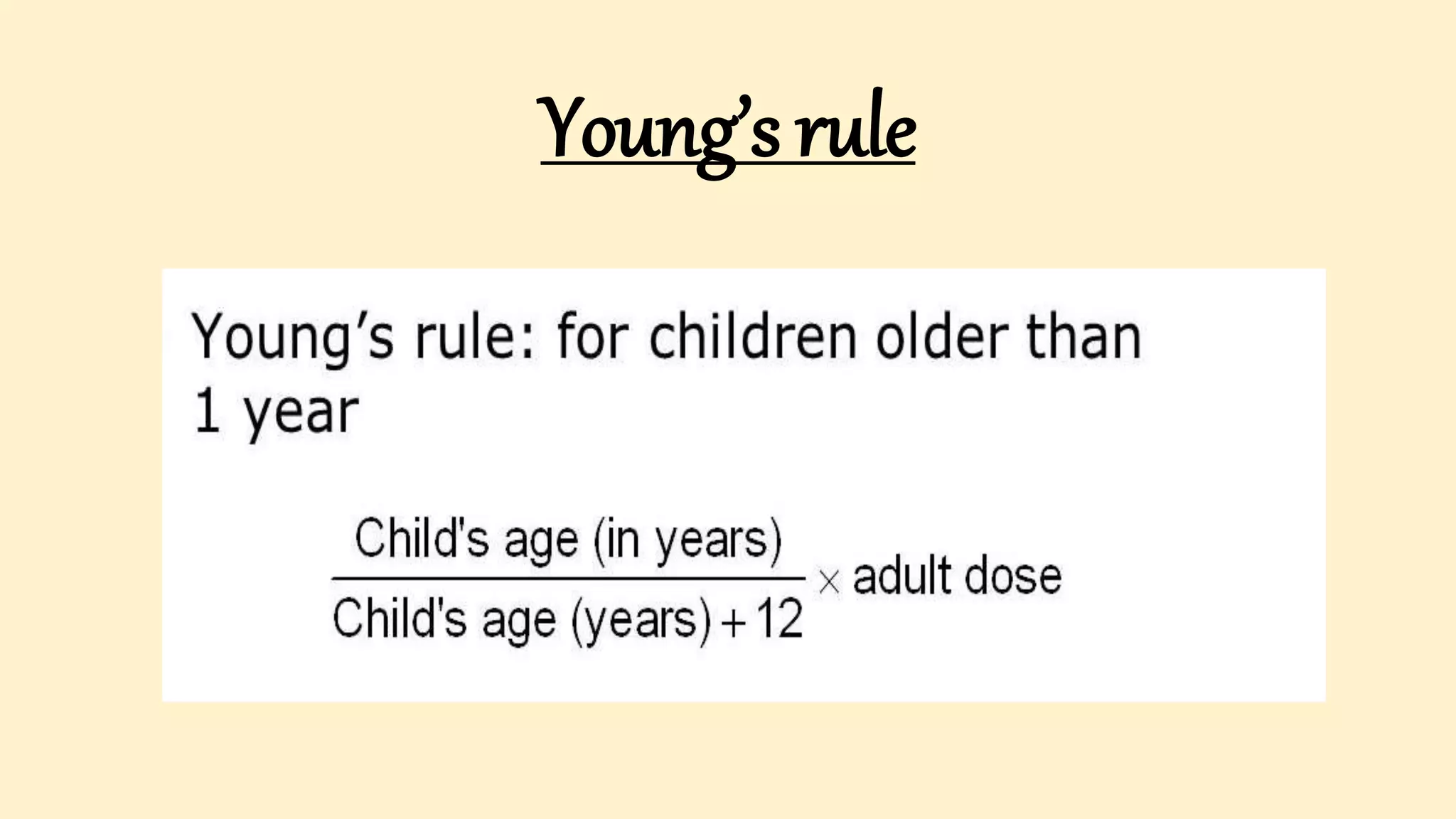
The document discusses the critical skill of drug calculations in pediatrics, emphasizing the importance for healthcare professionals to accurately determine medication dosages based on factors such as weight, age, and organ function. It covers essential terminology, pharmacokinetics, methods for calculating doses, and adjustments required for various patient populations, including infants and the elderly. Additionally, the document explains relevant formulas for computing body surface area and outlines factors that can influence drug action and effectiveness.
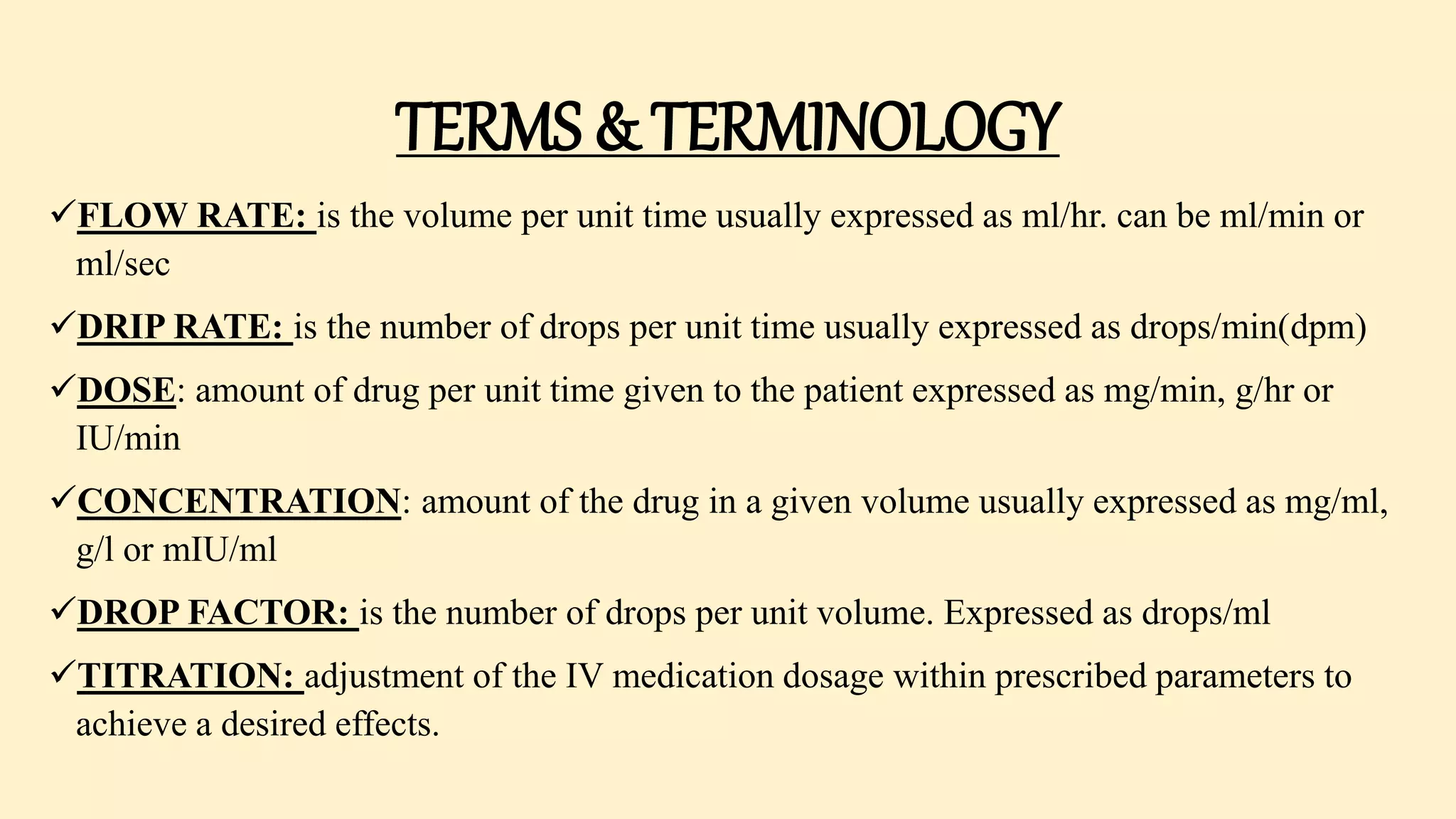









![•Body Surface Area (BSA) is very important in pediatric
drug dosage calculation.
There are two formulae that are generally used to calculate a
child’s BSA.
1. BSA= Sq. Root [(weight in kg * height in cm) ÷ 3600]
2. BSA= Sq. Root [(weight in pounds * height in inches) ÷
3131]](https://image.slidesharecdn.com/drugcalculations-211017103319/75/Pediatric-Drug-calculations-drug-calculation-formulas-24-2048.jpg)
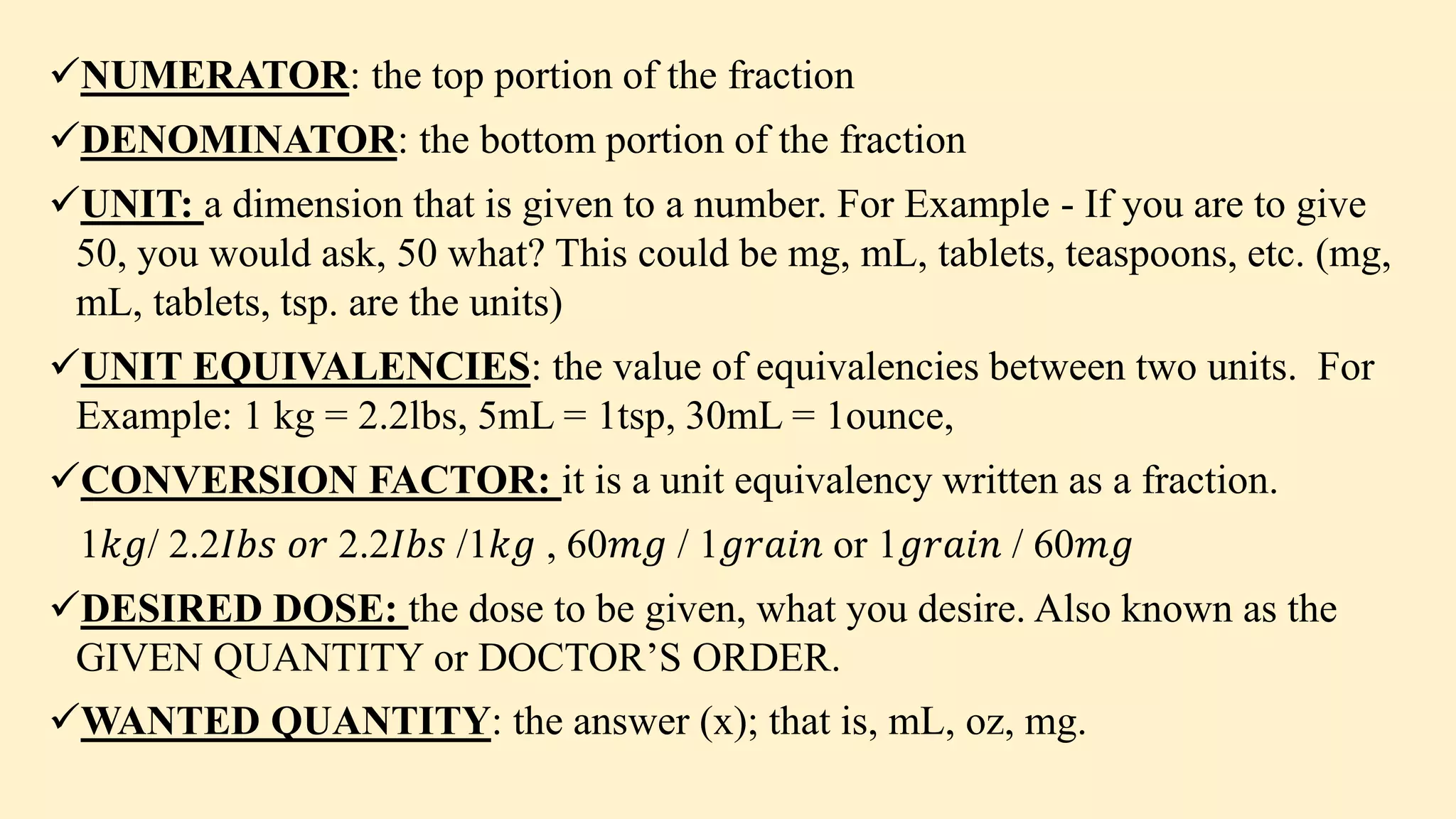
![Example:- Calculate the BSA of a child who weighs 65lbs and 5feet
8inches tall.
Weight= 65lb
Height= 5ft 8in
Convert 5ft to inches, then add it to 8in
1ft= 12in
5ft= 5*12= 60in
Height= 60 + 8= 68in
BSA= Sq. Root [(weight in pounds * height in inches) ÷ 3131]
BSA= Sq.root [(65*68)÷3131]
= sq.root [4420÷3131]
= sq.root [1.41]
= 1.19
BSA of the child is 1.19 sq meter](https://image.slidesharecdn.com/drugcalculations-211017103319/75/Pediatric-Drug-calculations-drug-calculation-formulas-25-2048.jpg)
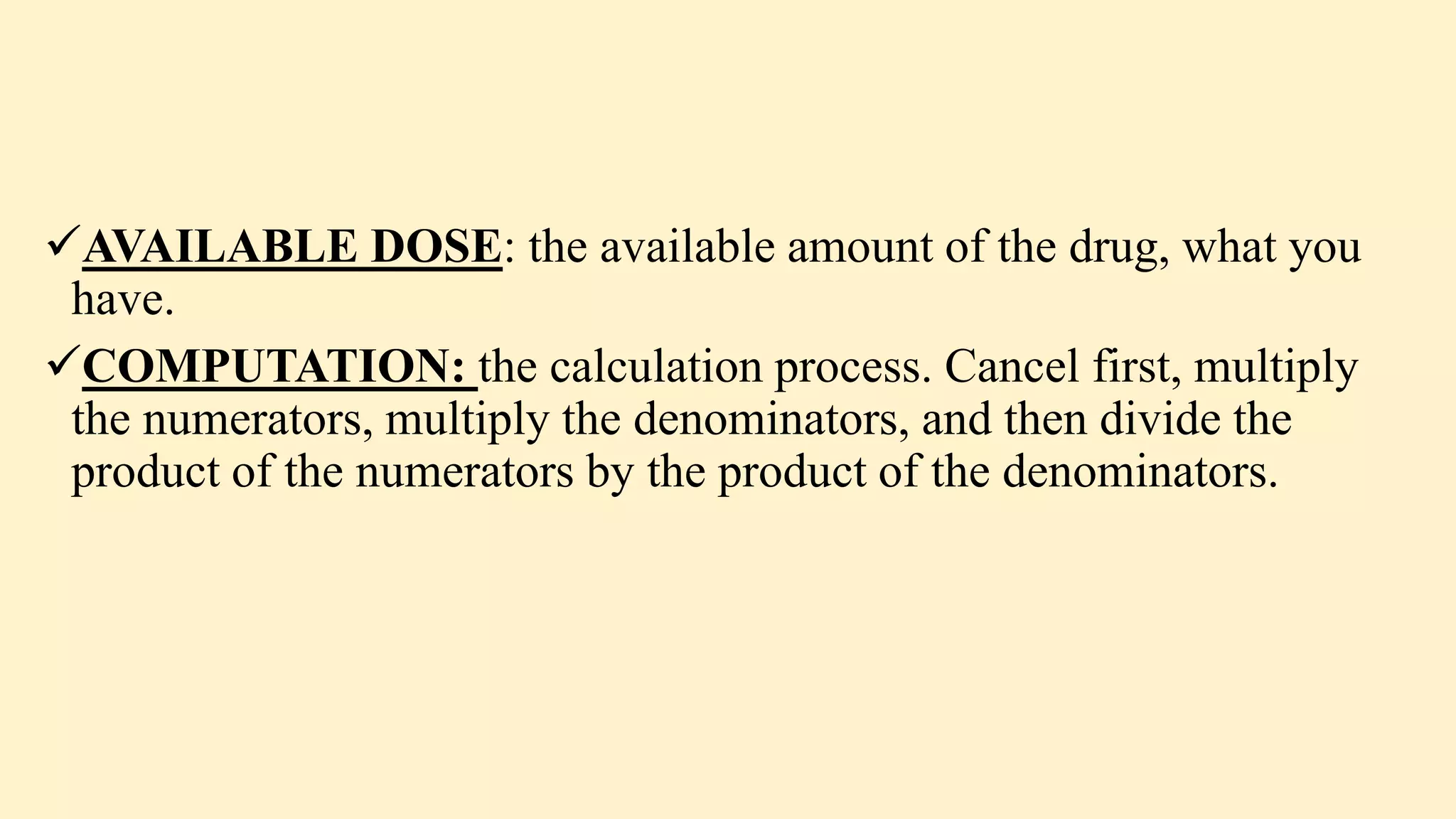
![Example 2:Calculate the BSA of a child who weighs 11.3kg and
75cm tall.
Weight= 11.3kg
Height= 75cm
BSA= Sq. Root [(weight in kg * height in cm) ÷ 3600]
= sq.root [(11.3*75)÷3600]
= sq.root [847.5÷3600]
= sq.root [0.24]
= 0.49
BSA of the child is 0.49 sq meter](https://image.slidesharecdn.com/drugcalculations-211017103319/75/Pediatric-Drug-calculations-drug-calculation-formulas-26-2048.jpg)