The document discusses the physiology of coronary blood flow and the microcirculation. Some key points include:
- Coronary blood flow is determined not only by proximal pressures but also by active compression and decompression of the microcirculation.
- Distal coronary pressure is influenced by both pressure transmitted from the aorta and pressure arising from the microcirculation.
- Fractional flow reserve (FFR) provides a measure of maximum achievable blood flow through a stenosis compared to a normal artery, indicating the functional significance of the stenosis.
- An FFR below 0.80 accurately identifies lesions causing ischemia, while a value above 0.80 reliably excludes ischemia.
































































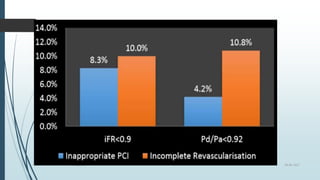
![ Assessment of the success of PCI [Class IIa, C]
•Evaluation of angina in patients without apparent agiographic stenosis [Class IIb, C]
28-06-2017FFR and iFR](https://image.slidesharecdn.com/ffr-170628145131/85/Ffr-66-320.jpg)