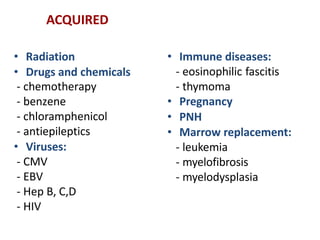
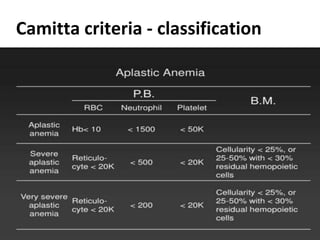
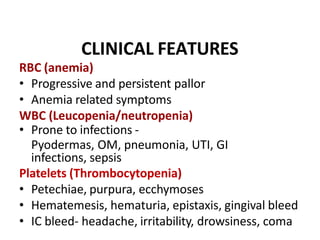
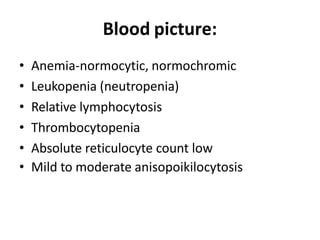
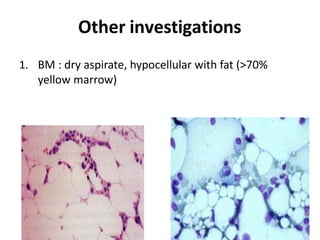
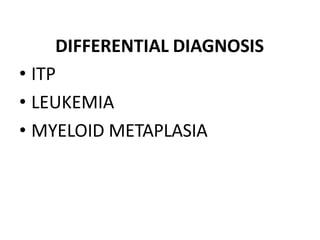
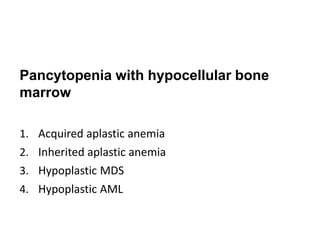
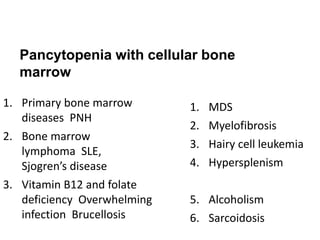
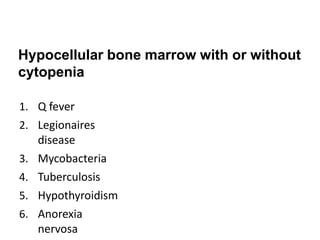
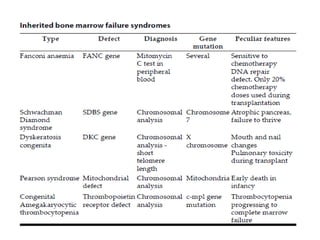
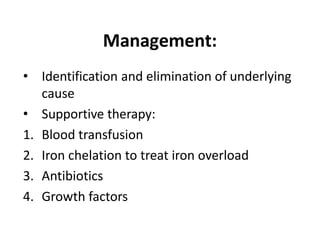
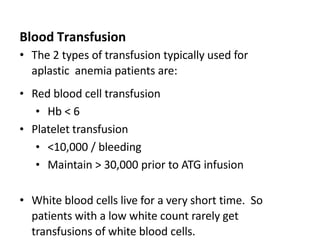
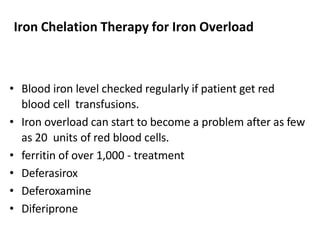
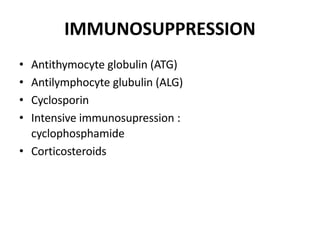
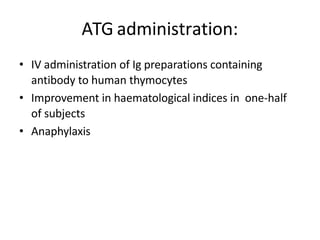
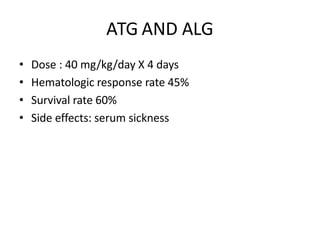
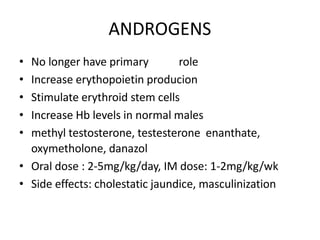
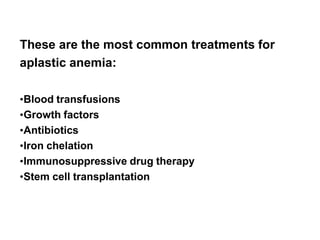
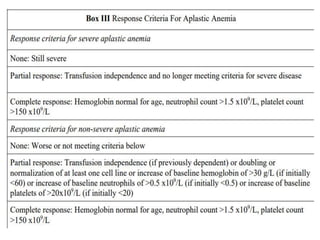
This document defines aplastic anemia and discusses its etiology, pathology, clinical features, diagnosis, differential diagnosis, and management. Aplastic anemia is a failure of two or more blood cell lines caused by hypoplasia or aplasia of the bone marrow. It can be hereditary or acquired through radiation, drugs, viruses, or immune diseases. Clinically, it presents with pancytopenia and increased risk for infections and bleeding. Treatment involves blood transfusions, antibiotics, growth factors, immunosuppressive drugs, and stem cell transplantation.
![Aplastic Anemia
Download more documents and slide shows on The Medical Post [ www.themedicalpost.net ]
Dr. Kalpana Malla
MD Pediatrics
Manipal Teaching Hospital](https://image.slidesharecdn.com/aplasticanemia-230928123555-af4567a1/75/aplastic-anemia-pptx-1-2048.jpg)


![Thank you
Download more documents and slide shows on The
Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/aplasticanemia-230928123555-af4567a1/85/aplastic-anemia-pptx-35-320.jpg)