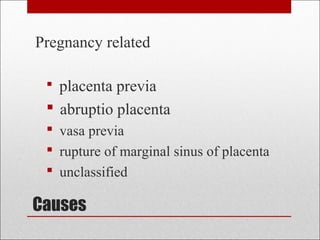
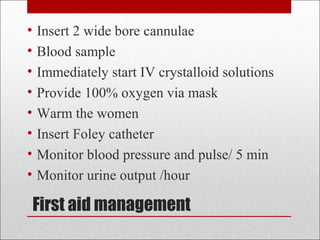
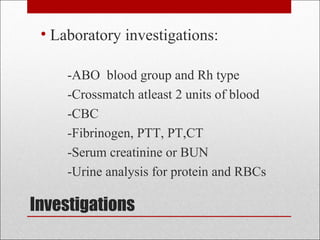
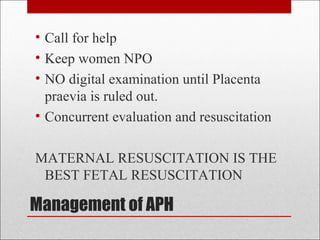
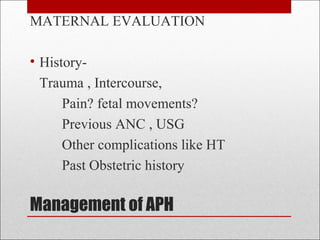
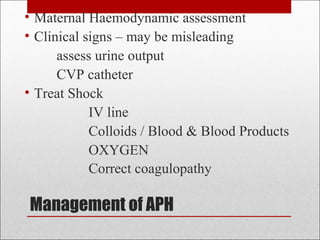
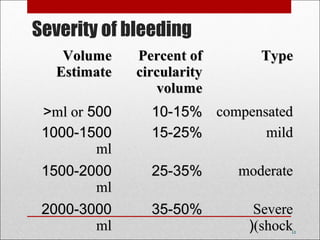
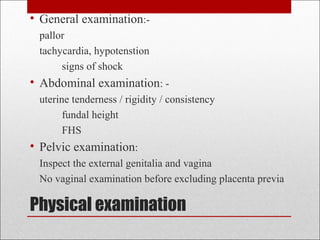
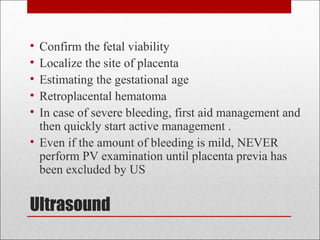
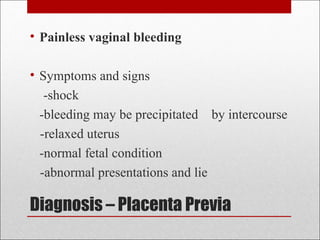
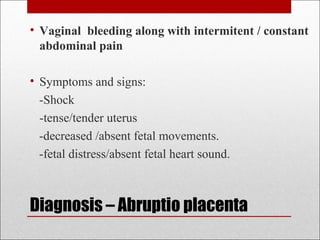
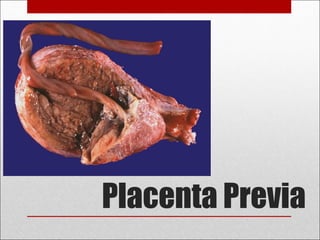
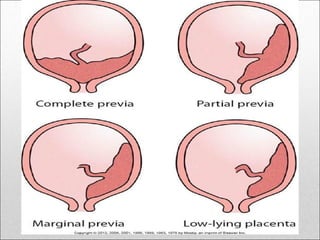
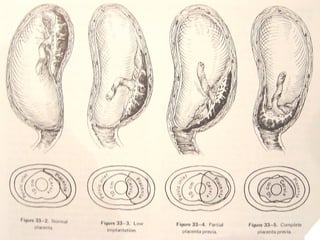
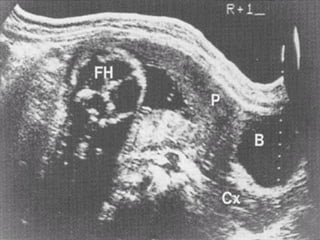
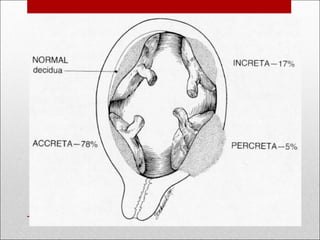
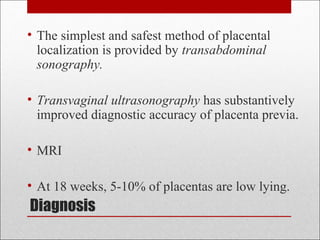
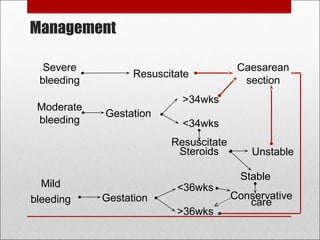
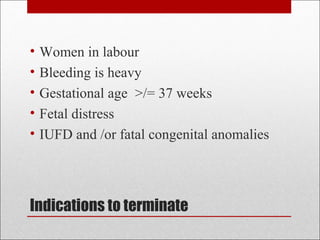
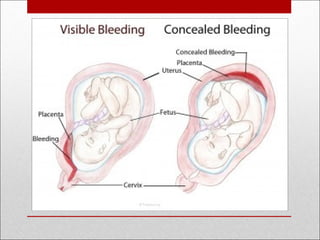
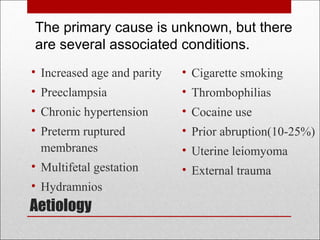
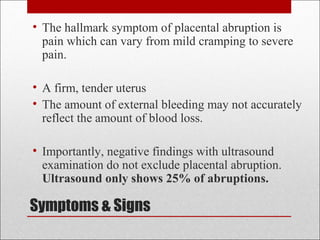
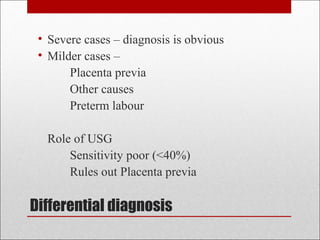
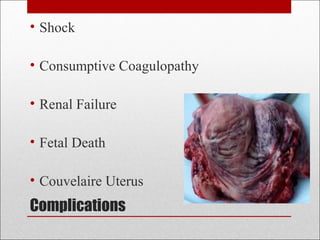
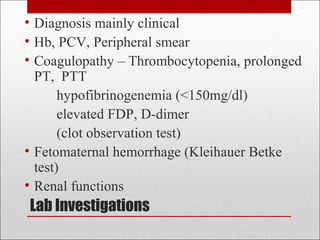
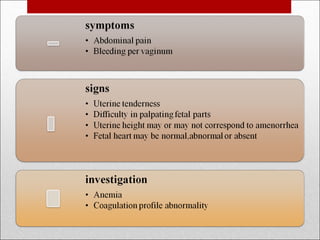
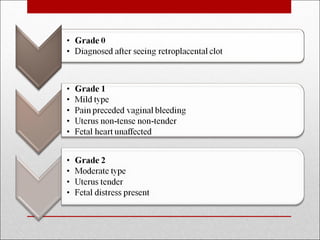
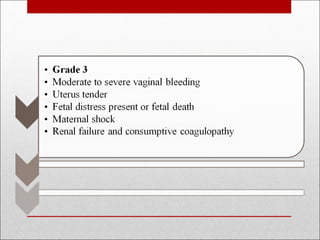
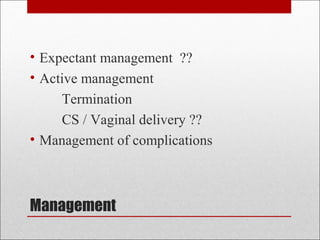
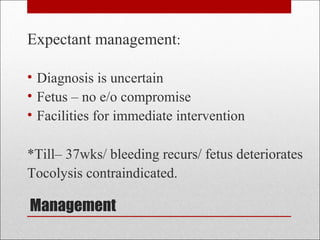
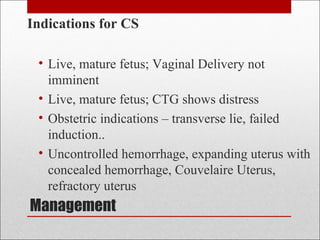
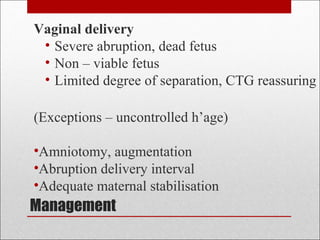
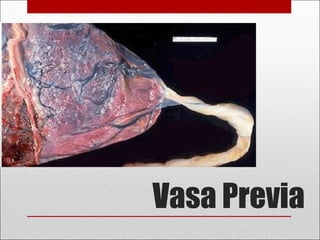
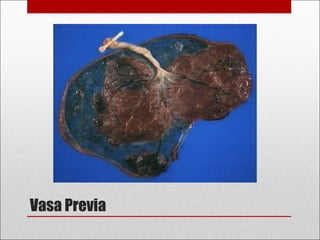
Antepartum hemorrhage, or bleeding during pregnancy, is a medical emergency that can have serious consequences. The most common causes are placenta previa, abruptio placenta, and vasa previa. In placenta previa, the placenta covers all or part of the cervix, which can cause painless bleeding. Abruptio placenta occurs when the placenta separates prematurely from the uterus, often causing abdominal pain and bleeding. Vasa previa involves blood vessels running through the membranes near the cervix, which can rupture during labor. Immediate medical care is needed to stabilize the mother and determine the cause through ultrasound and other tests in order to guide management