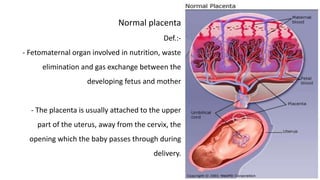
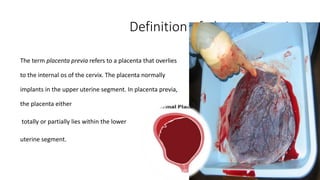
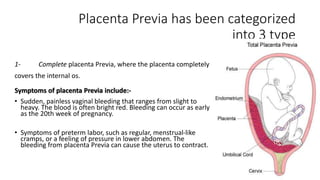
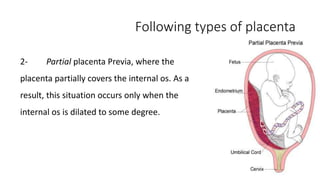
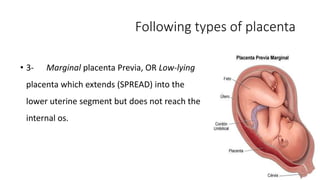
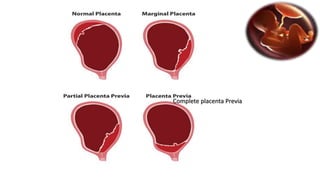
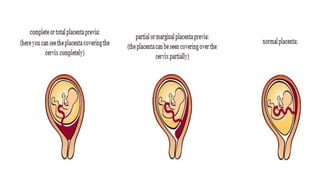
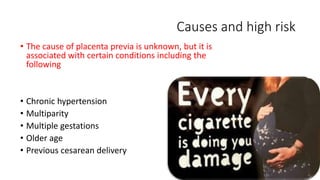
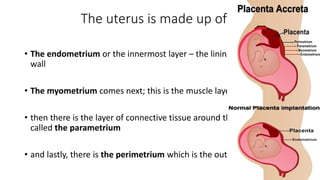
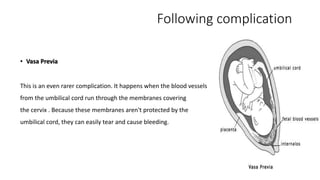
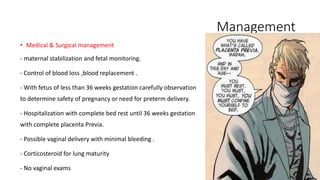
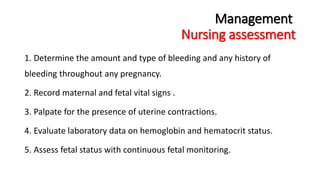
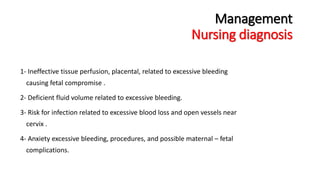
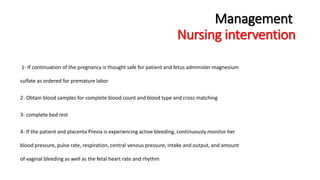
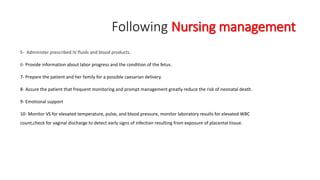
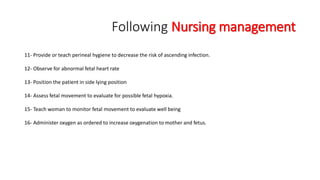
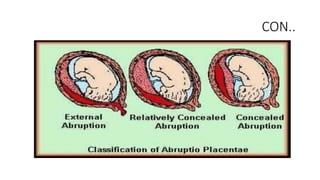
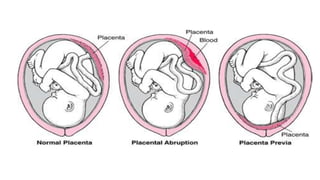
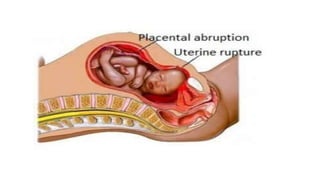
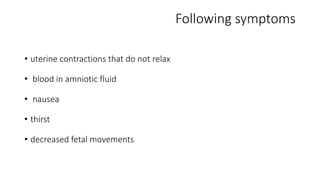
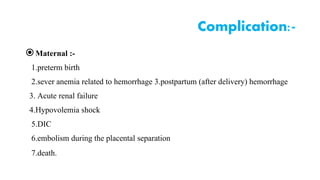
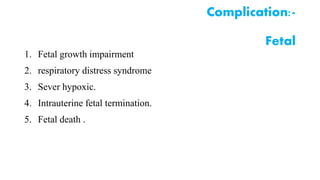
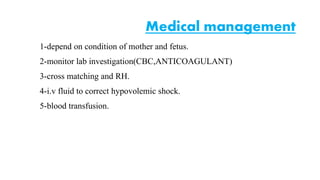
Placental abruption and placenta previa are two common causes of bleeding in late pregnancy. Placental abruption occurs when the placenta separates from the inner wall of the uterus before delivery. It can cause pain and vaginal bleeding. Placenta previa is when the placenta lies low in the uterus, covering all or part of the cervical opening. It typically causes painless vaginal bleeding. Both conditions can lead to complications for the mother like hemorrhage, shock, and infection or complications for the baby like low birth weight or stillbirth. Treatment depends on gestational age and severity of bleeding but may involve bed rest, monitoring, blood transfusions, or delivery via c-section