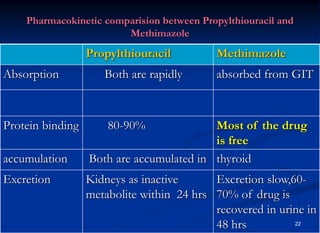
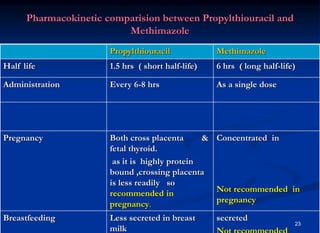
This document discusses drugs used to treat hyperthyroidism. It describes the mechanisms and effects of common drug classes including thioamides like methimazole and propylthiouracil which inhibit thyroid hormone synthesis; iodides which block hormone production and conversion; radioactive iodine which destroys thyroid tissue; and beta blockers which relieve symptoms. Adverse effects, clinical uses, and special considerations for conditions like Graves' disease and pregnancy are covered.