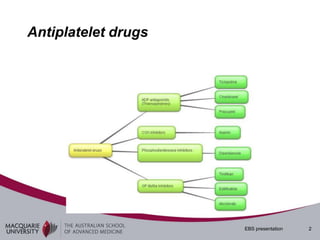
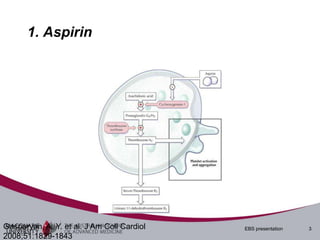
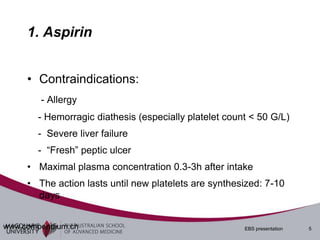
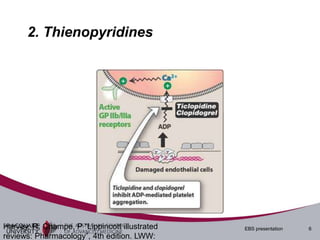
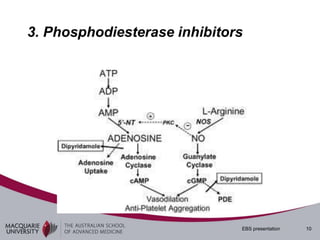
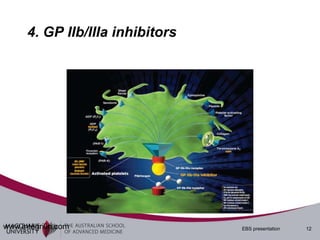
1. This document discusses various antiplatelet drugs including aspirin, Plavix, and GP IIb/IIIa inhibitors. It summarizes their mechanisms of action, indications, contraindications, and durations of effect.
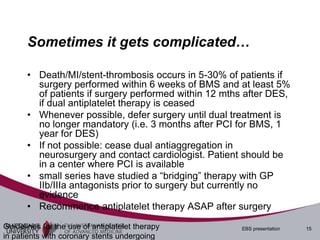
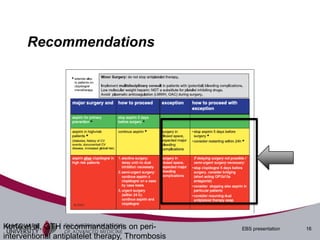
2. In neurosurgery, antiplatelet drugs cannot be reversed as their effects are irreversible. Surgery may be delayed if a patient needs dual antiplatelet therapy following stent placement.
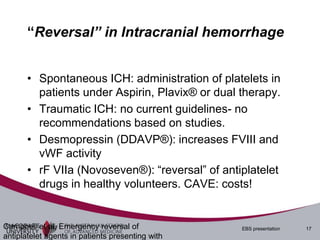
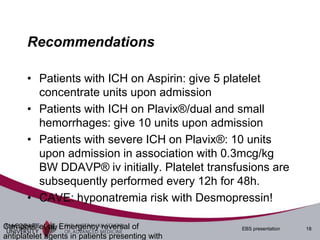
3. For intracranial hemorrhage in patients on antiplatelets, platelet transfusions are recommended along with potentially Desmopressin or rF VIIa in more severe cases to attempt reversal of effects. Close monitoring is needed due to bleeding risks.