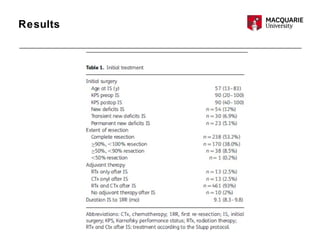
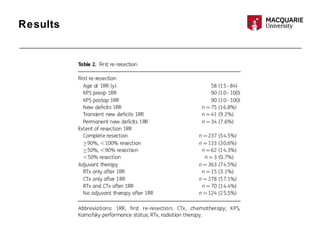
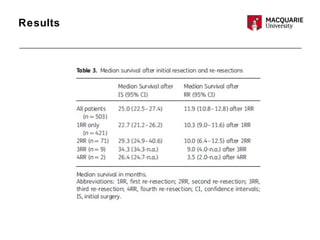
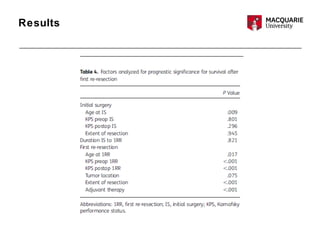
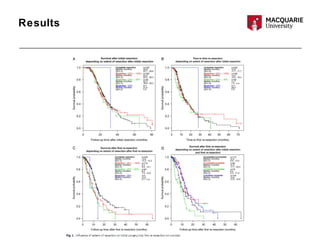
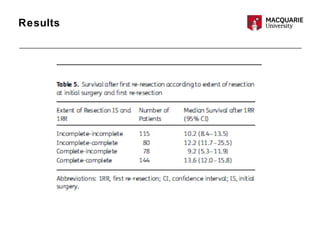
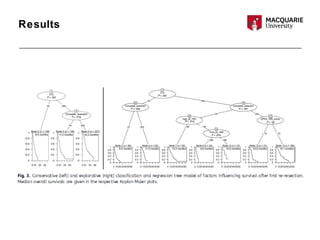
This multicenter study examined 503 patients with recurrent glioblastomas who underwent surgical resection. It found that aggressive surgical resection of recurrent glioblastomas, when followed by adjuvant therapy, was associated with increased overall survival. Specifically, survival was longer for patients who were younger, had a higher Karnofsky performance status, underwent a more extensive resection, and had a longer time between initial diagnosis and recurrence. However, the study had limitations as a retrospective analysis subject to selection bias. Repeat resection improved survival, but its benefits compared to nonsurgical therapy require further prospective evaluation.