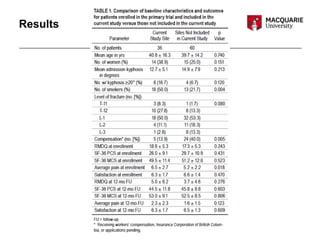
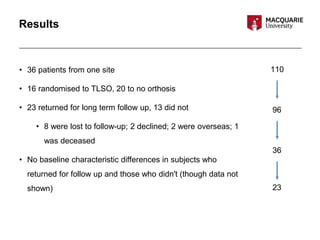
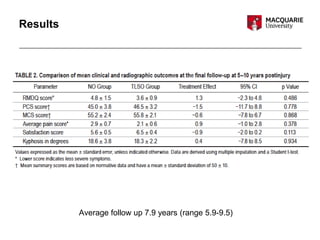
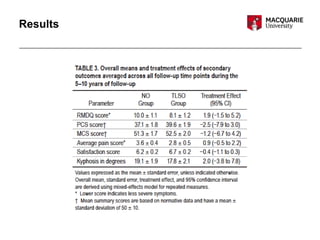
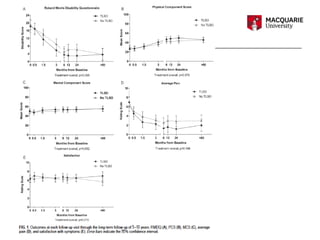
This document summarizes a journal club discussion on a study comparing orthosis versus no orthosis for treatment of thoracolumbar burst fractures. The study was a follow up of patients from 5-10 years after an initial randomized trial. It found that at long term follow up, patients treated with early mobilization without orthosis had similar functional outcomes and pain levels as those initially treated with a thoracolumbar orthosis brace. However, the follow up study had a small sample size and high risk of bias.