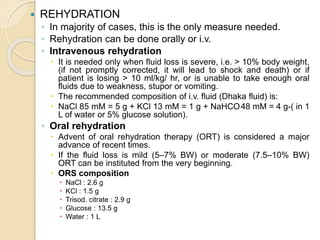
This document discusses antidiarrheal drugs and their use and mechanisms. It begins by defining diarrhea and describing potential causes related to electrolyte and water balance or intestinal inflammation. Treatment involves rehydration, either orally or intravenously depending on severity, as well as drug therapy when needed. Specific antimicrobials may be used for infectious causes like cholera, while probiotics and drugs for inflammatory bowel disease are also discussed. Finally, nonspecific antidiarrheal drugs that work by absorption, decreasing secretion, or reducing motility are outlined, including examples like loperamide, codeine, and racecadotril.