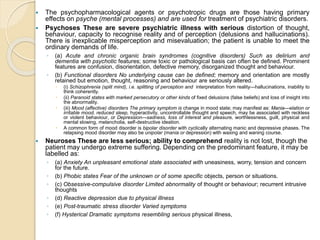
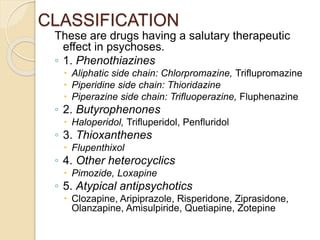
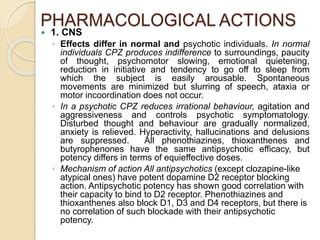
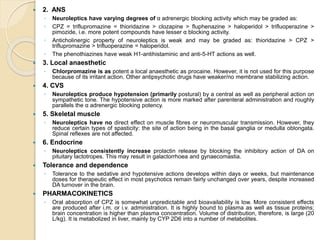
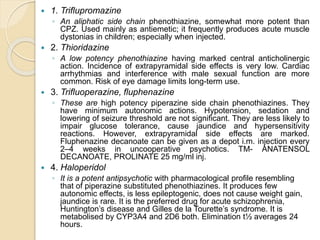
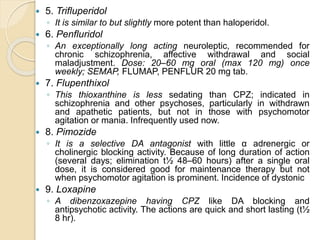
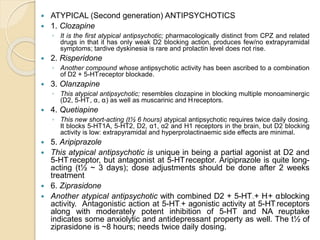
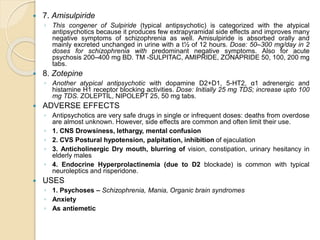
This document discusses tranquilizers and antipsychotic drugs. It begins by defining tranquilizers as drugs used to treat anxiety, fear, and mental disturbances by reducing tension and anxiety. It then classifies psychotropic drugs into different categories based on their effects: antipsychotics, antimanic mood stabilizers, antidepressants, anxiolytics, and psychotomimetics. The majority of the document focuses on antipsychotic drugs, describing their pharmacological actions, classifications, examples of different drug classes, and their adverse effects. It provides details on both typical and atypical antipsychotics, and concludes by stating their common uses in treating psychoses, schizophrenia, mania, and organic brain syndromes.