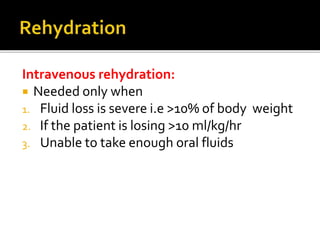
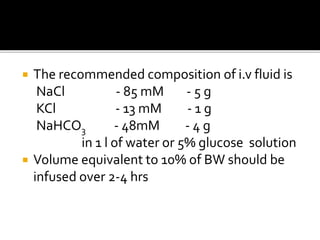
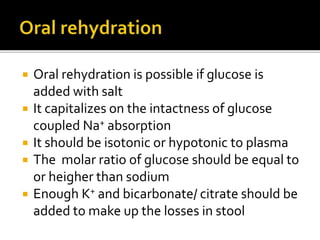
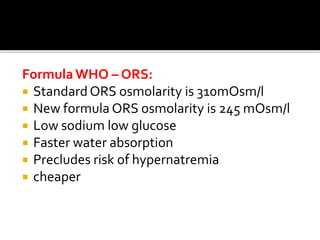
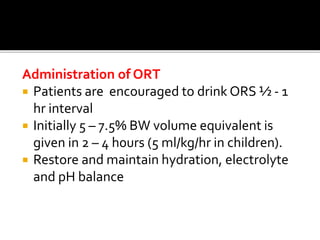
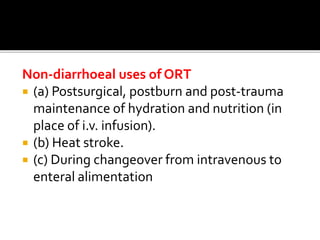
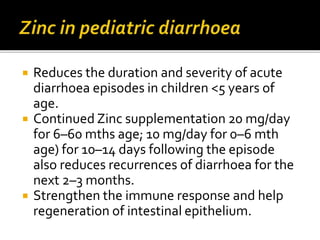
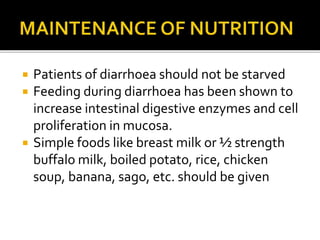
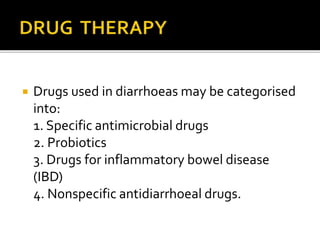
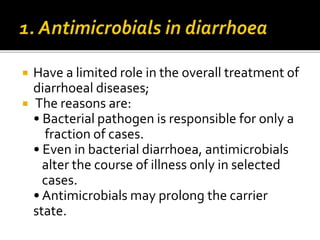
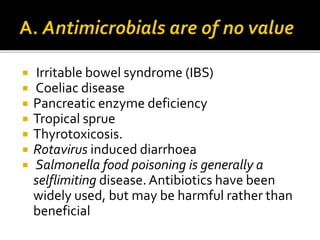
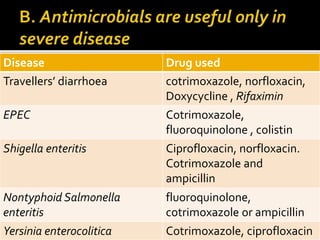
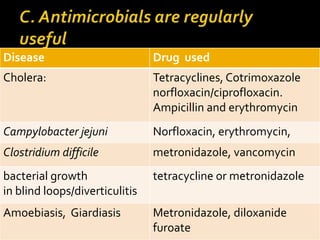
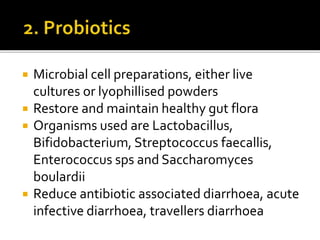
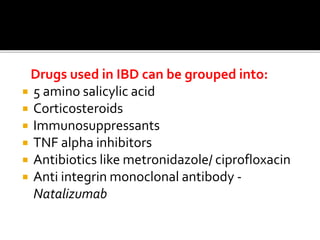
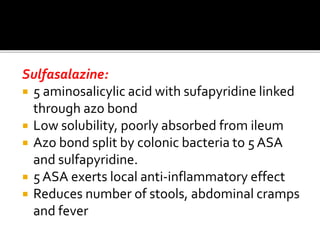
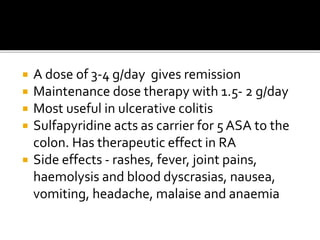
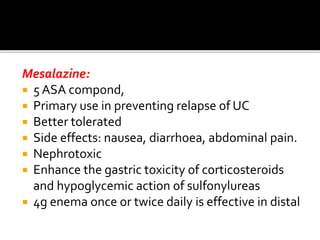
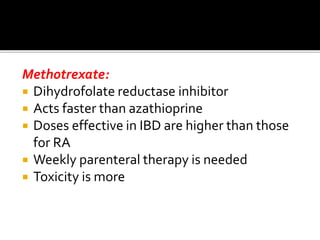
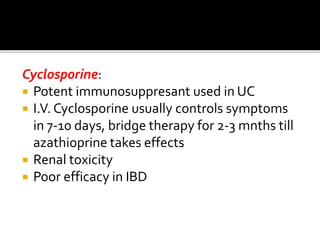
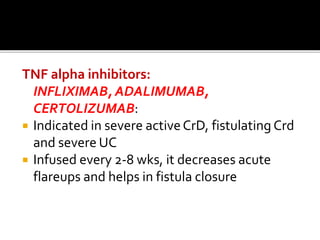
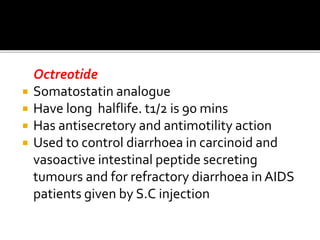
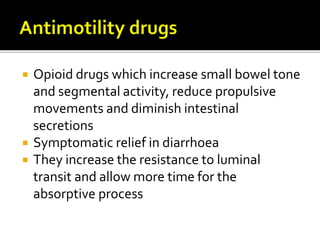
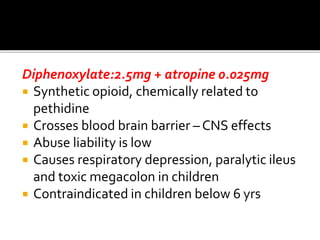
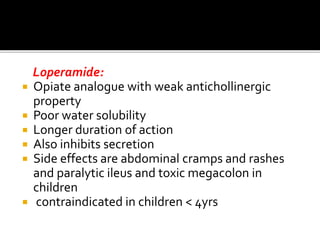
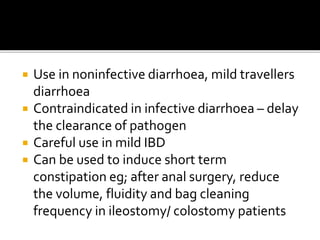
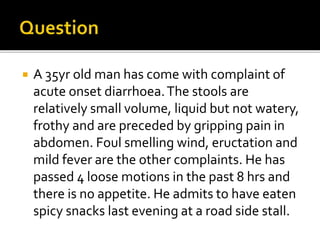
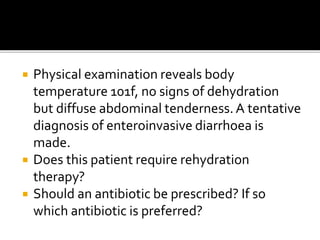
This document provides information on the definition, causes, pathology, treatment and management of diarrhoea. It discusses oral rehydration therapy and intravenous fluid replacement. It covers specific infectious causes of diarrhoea and appropriate antibiotic use. The document also outlines management of inflammatory bowel diseases and use of antimotility drugs and symptomatic treatments.