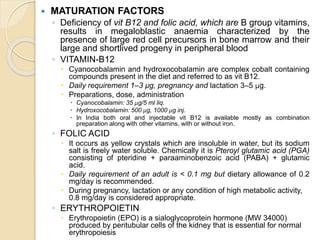
This document discusses hematinic drugs used to treat anemia. It describes three main categories of hematinics: iron supplements, which come in various oral and injectable forms; vitamin B12 and folic acid, which are important for red blood cell maturation; and erythropoietin, a hormone produced in the kidney that is essential for red blood cell production. Side effects of oral iron supplements include gastrointestinal issues. Parenteral iron is recommended when oral iron is not absorbed or tolerated. Vitamin B12 and folic acid deficiencies can cause megaloblastic anemia.