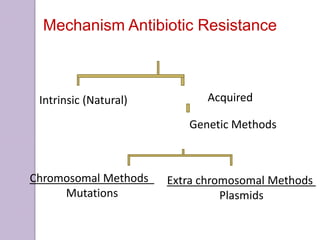
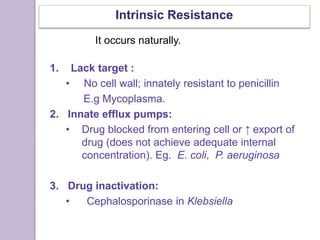
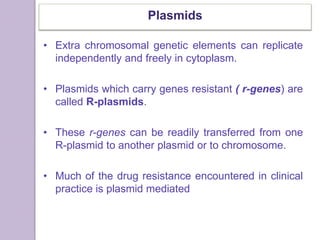
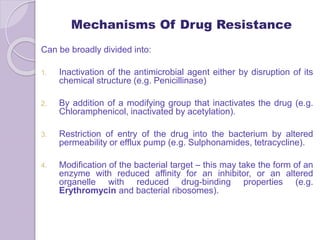
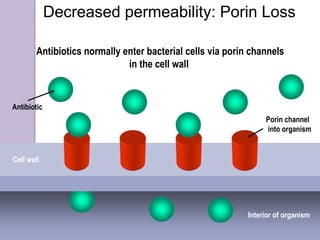
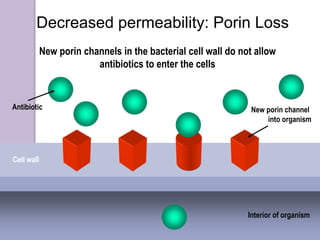
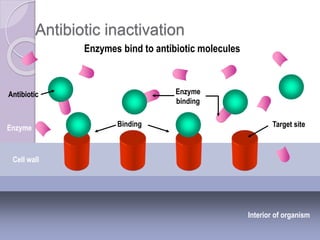
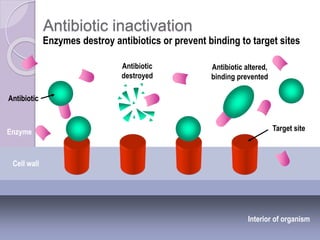
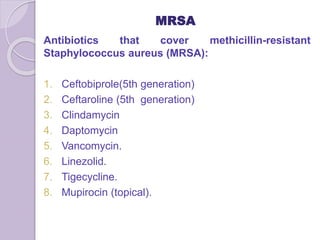
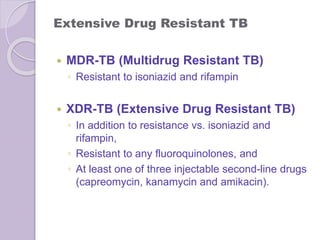
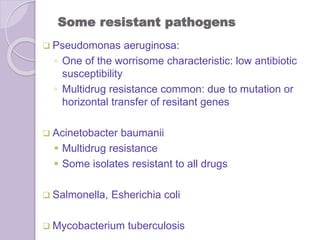
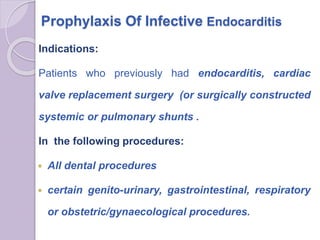
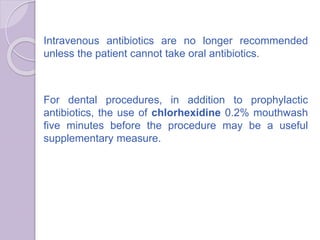
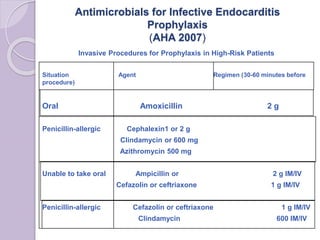
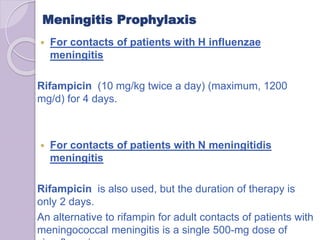
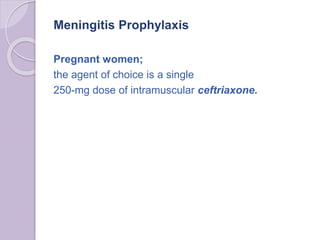
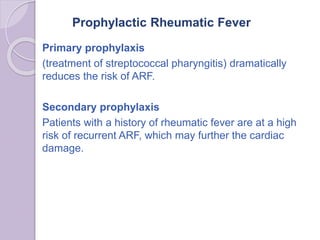
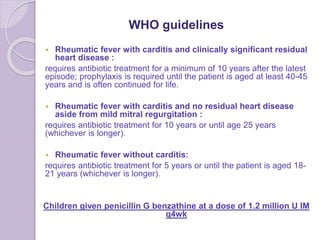
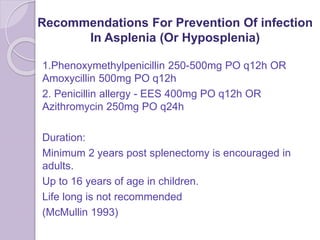
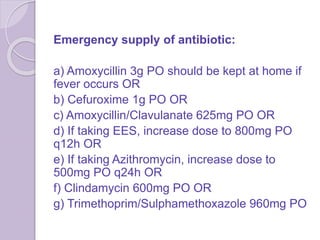
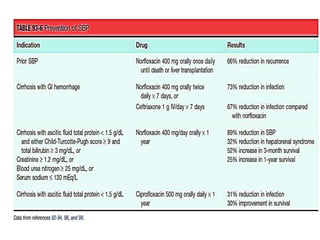
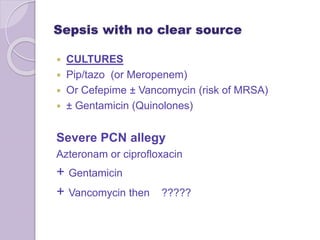
This document discusses various types of antibiotic prophylaxis. It outlines recommendations for prophylaxis of infective endocarditis, which involves administering antibiotics prior to certain medical procedures for at-risk patients. It also mentions prophylactic preoperative antibiotics, prophylactic treatment for rheumatic fever, prevention of spontaneous bacterial peritonitis, meningitis prophylaxis, and prophylaxis for cellulitis. Common antibiotics used for different types of prophylaxis are listed, along with their dosages and administration routes. Mechanisms of antibiotic resistance in bacteria are summarized, including both intrinsic and acquired resistance.