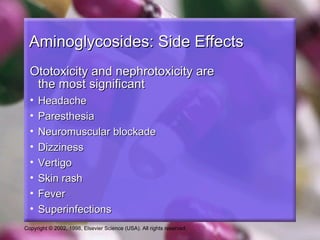
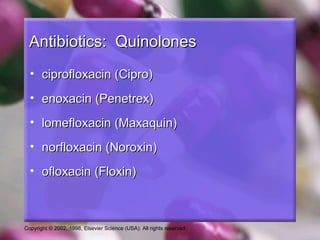
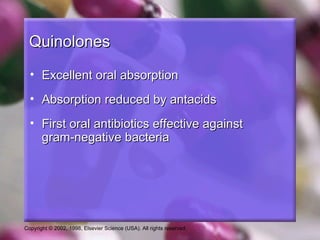
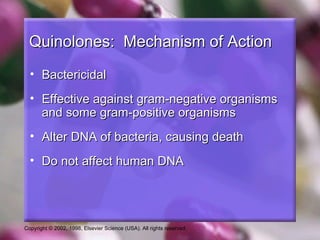
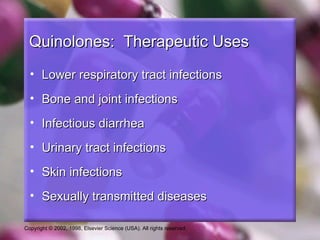
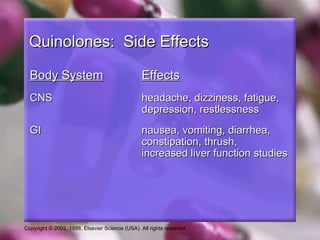
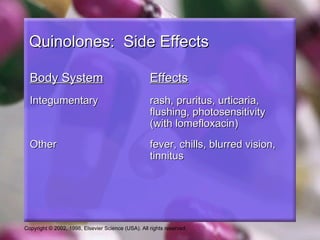
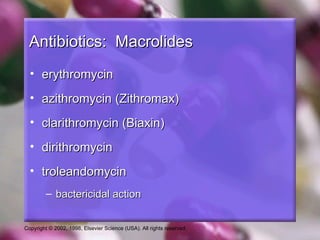
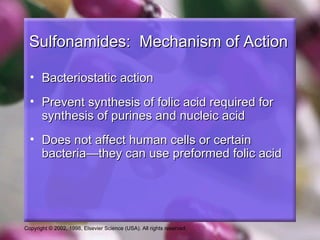
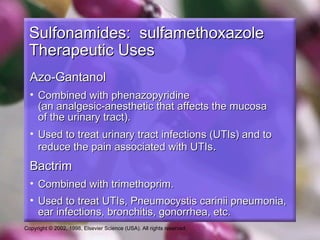
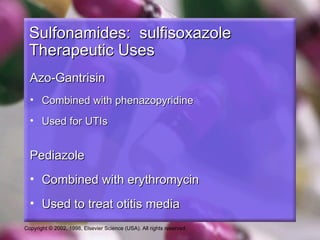
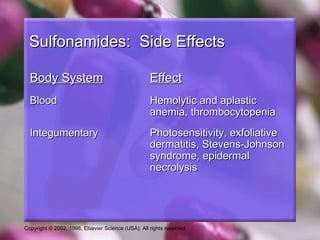
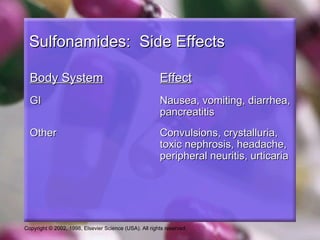
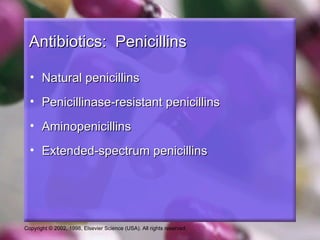
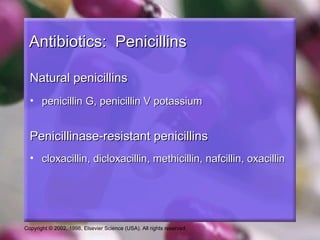
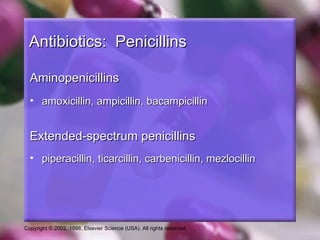
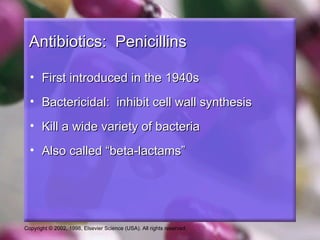
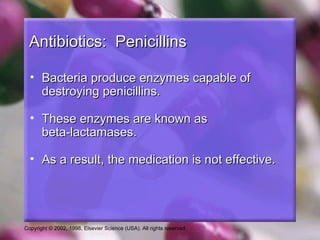
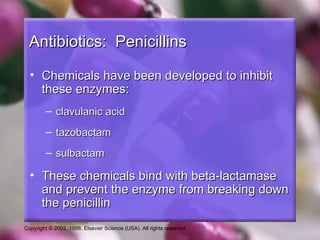
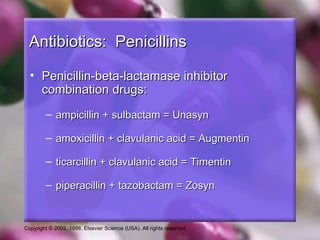
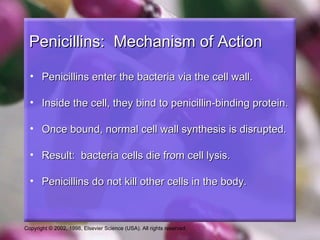
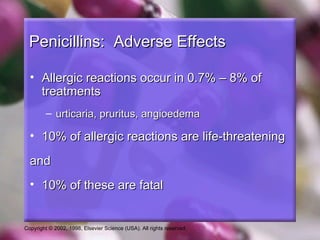
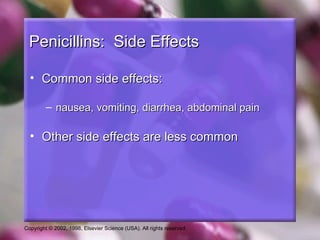
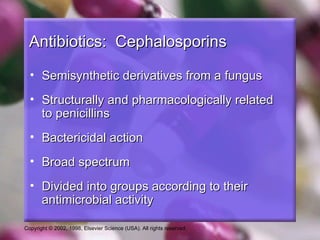
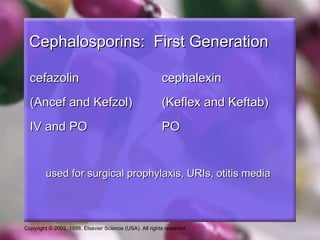
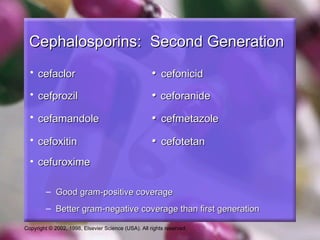
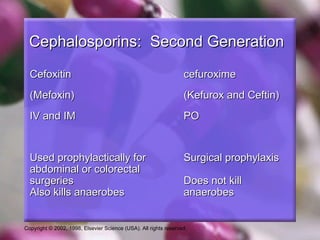
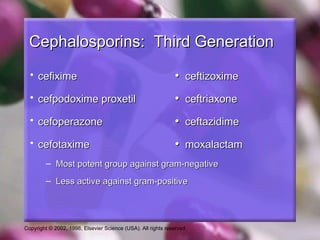
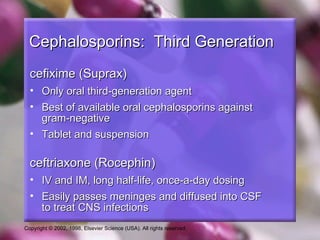
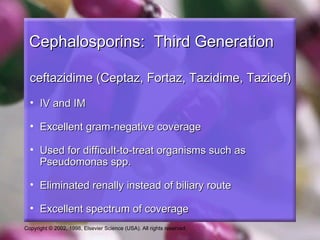
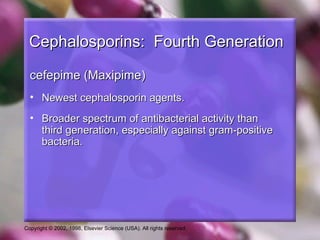
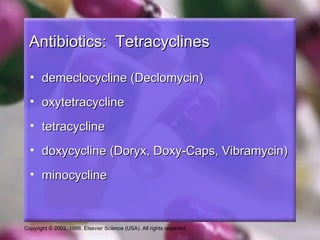
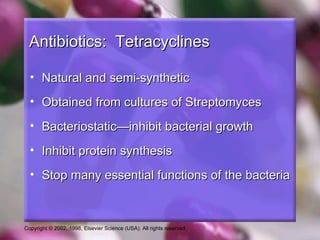
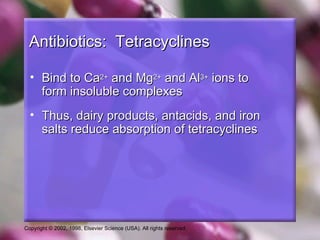
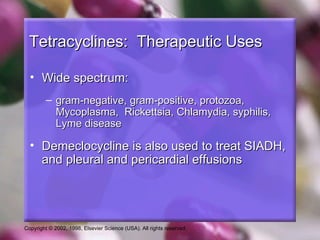
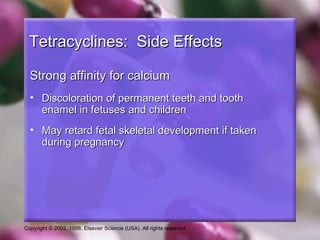
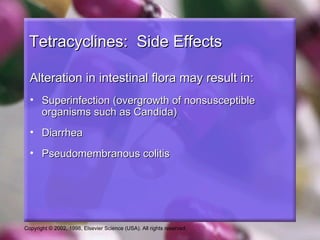
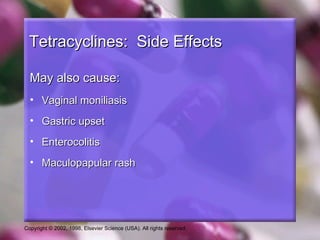
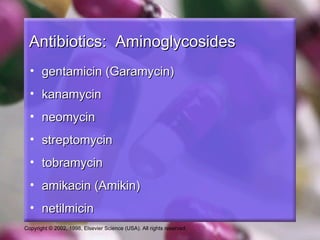
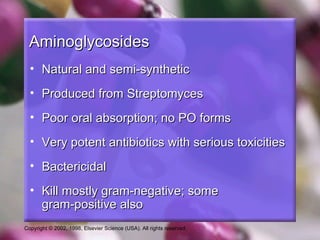
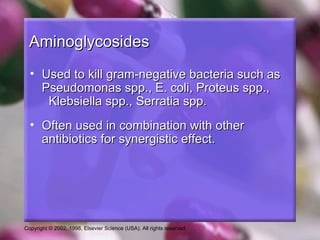
The document discusses several classes of anti-infective agents including antibiotics such as sulfonamides, penicillins, cephalosporins, tetracyclines, aminoglycosides, and quinolones. It provides details on the mechanisms of action, therapeutic uses, and common side effects of these antibiotic classes.


![Aminoglycosides
• Three most common (systemic): gentamicin,
tobramycin, amikacin
• Cause serious toxicities:
– Nephrotoxicity (renal failure)
– Ototoxicity (auditory impairment and vestibular
[eighth cranial nerve])
• Must monitor drug levels to prevent toxicities
Copyright © 2002, 1998, Elsevier Science (USA). All rights reserved.](https://image.slidesharecdn.com/38-antibiotics-120605125948-phpapp02/85/Antibiotics-43-320.jpg)