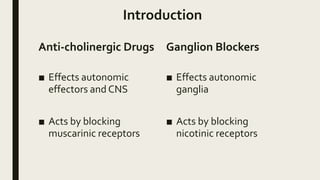
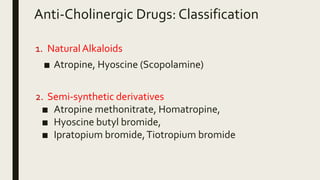
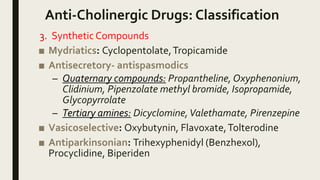
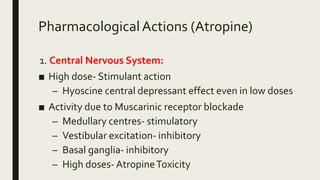
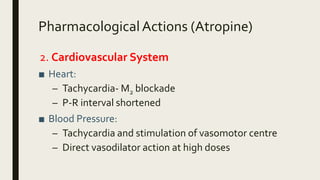
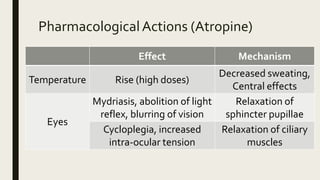
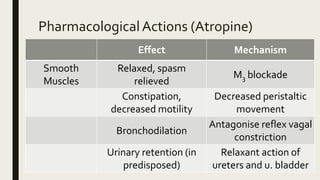
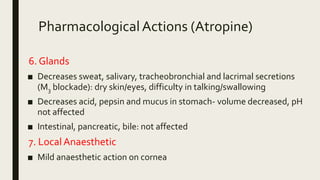
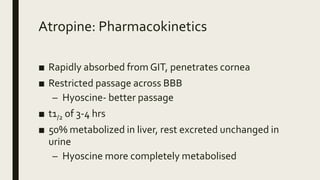
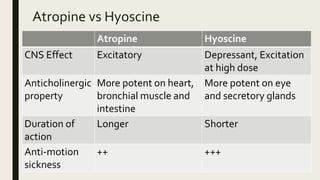
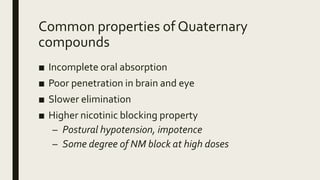
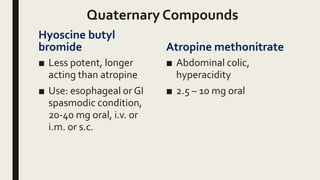
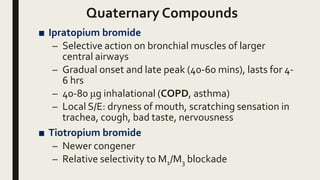
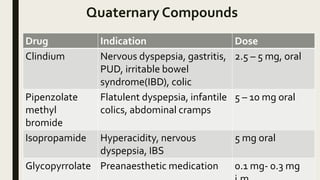
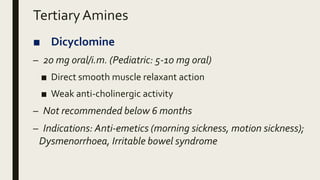
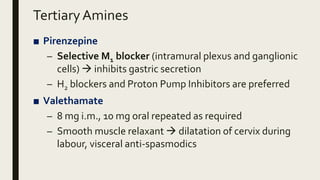
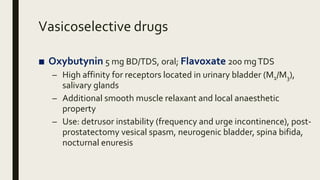
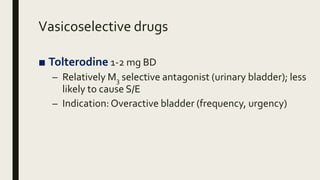
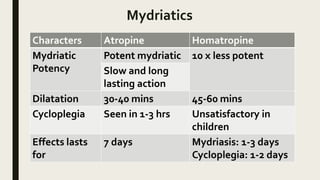
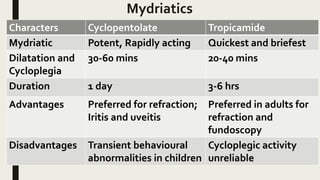
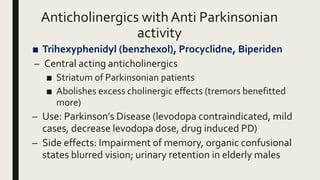
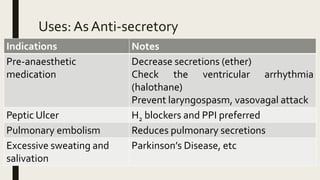
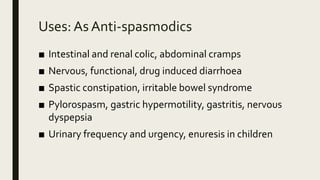
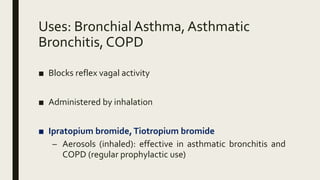
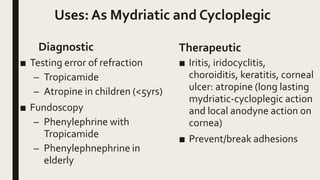
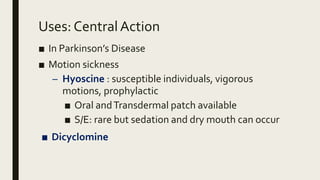
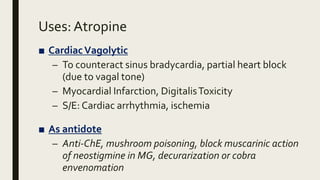
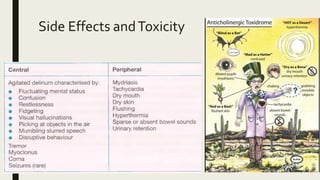
This document provides information about anti-cholinergic drugs, including their classification, mechanisms of action, pharmacokinetics, and uses. It discusses how anti-cholinergic drugs work by blocking muscarinic and nicotinic receptors. The main classes covered are natural alkaloids like atropine and hyoscine, semi-synthetic derivatives, synthetic compounds, and ganglion blockers. Key uses of these drugs include as antisecretory agents, bronchodilators, mydriatics, and for treating Parkinson's disease and overactive bladder. Common side effects result from their anticholinergic effects such as dry mouth, blurred vision, constipation, and urinary retention.