This document discusses the nervous system and the roles of acetylcholine and antimuscarinic agents. It covers:
- The central and peripheral nervous systems and their roles in receiving stimuli and initiating responses.
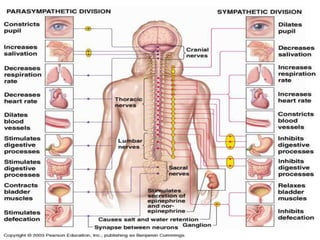
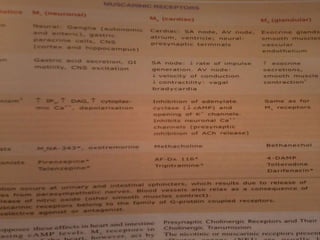
- Acetylcholine as the predominant neurotransmitter in the parasympathetic nervous system.
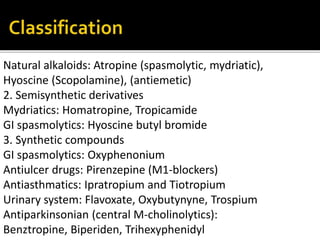
- Common antimuscarinic agents like atropine that work by blocking muscarinic receptors to inhibit parasympathetic functions.
- The clinical uses of antimuscarinic agents in various systems of the body like the eye, respiratory and gastrointestinal systems.
- Important side effects of antimuscarinic overdose.







![50
100
150
200
A B C D1 min
ATROPINE BLOCKS
M-EFFECTS OF ACH
Bloodpressure[mmHg]
ACh
2 mcg i.v.
ACh
50 mcg
ACh
50 mcg
ACh
5 mg
M-
effect
M-
effect
N-
effect
Atropine
2 mg i.v.
ACh](https://image.slidesharecdn.com/classanticholinergicdrugs-150519053206-lva1-app6891/85/Class-anticholinergic-drugs-12-320.jpg)























