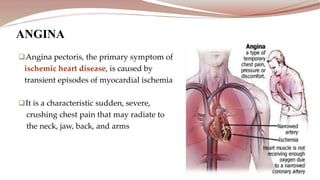
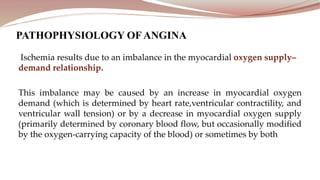
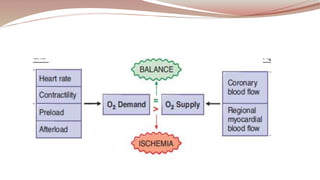
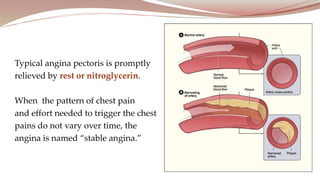
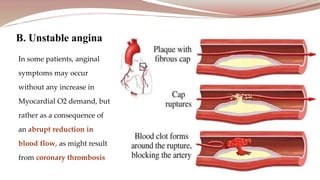
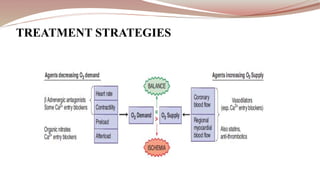
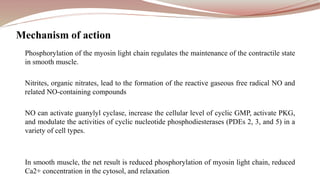
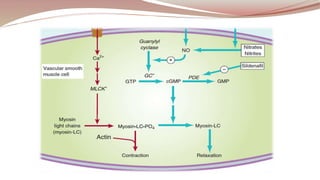
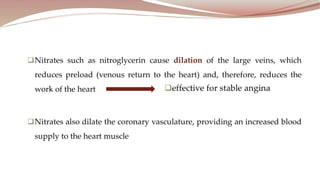
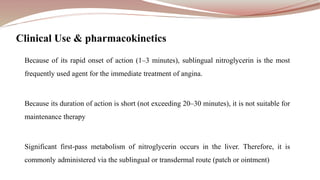
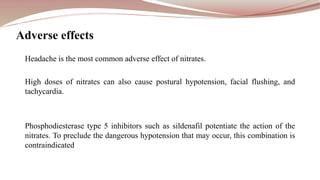
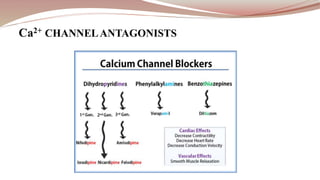
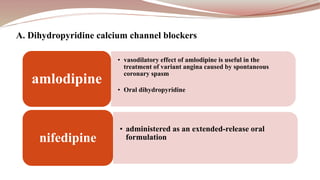
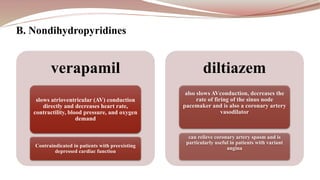
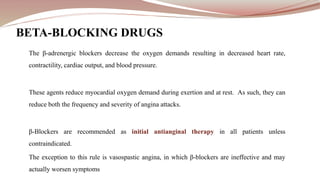
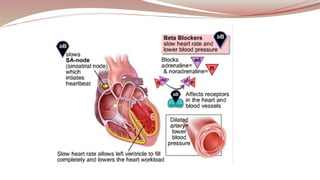
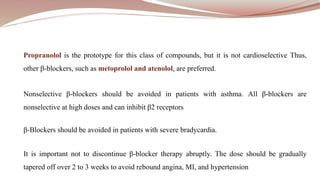
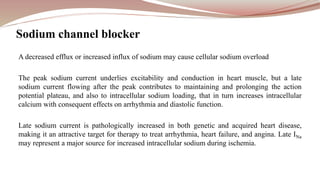
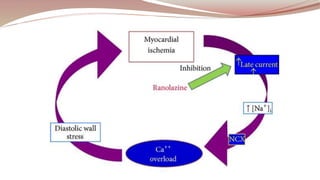
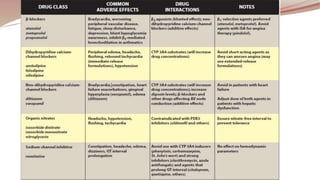
Angina pectoris is caused by transient episodes of myocardial ischemia due to an imbalance in the myocardial oxygen supply-demand relationship. There are three main types of angina: stable angina, which is triggered by exertion and relieved by rest; unstable angina, which occurs at rest and is a medical emergency; and Prinzmetal angina, which occurs due to coronary artery spasm. Treatment strategies for angina include nitrates like nitroglycerin which relieve symptoms rapidly, calcium channel blockers which prevent calcium entry and relax blood vessels, beta blockers which reduce the heart's oxygen demand, and ranolazine which inhibits sodium channels to reduce the heart's work.