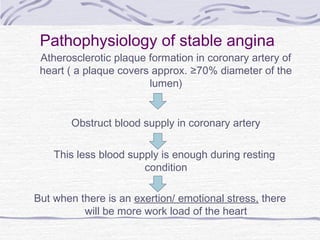
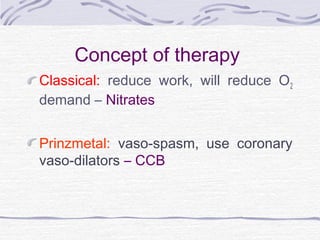
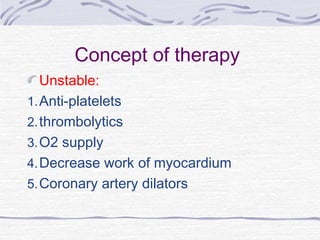
Angina pectoris is defined as transient chest pain due to cardiac ischemia, presenting in various forms such as stable, unstable, and variant angina. The condition is increasingly recognized as a significant public health concern, with millions affected and a high incidence rate, particularly among older populations and those with specific risk factors. Management strategies focus on symptom relief and prevention of myocardial infarction through pharmacologic and non-pharmacologic therapies, including lifestyle modifications.