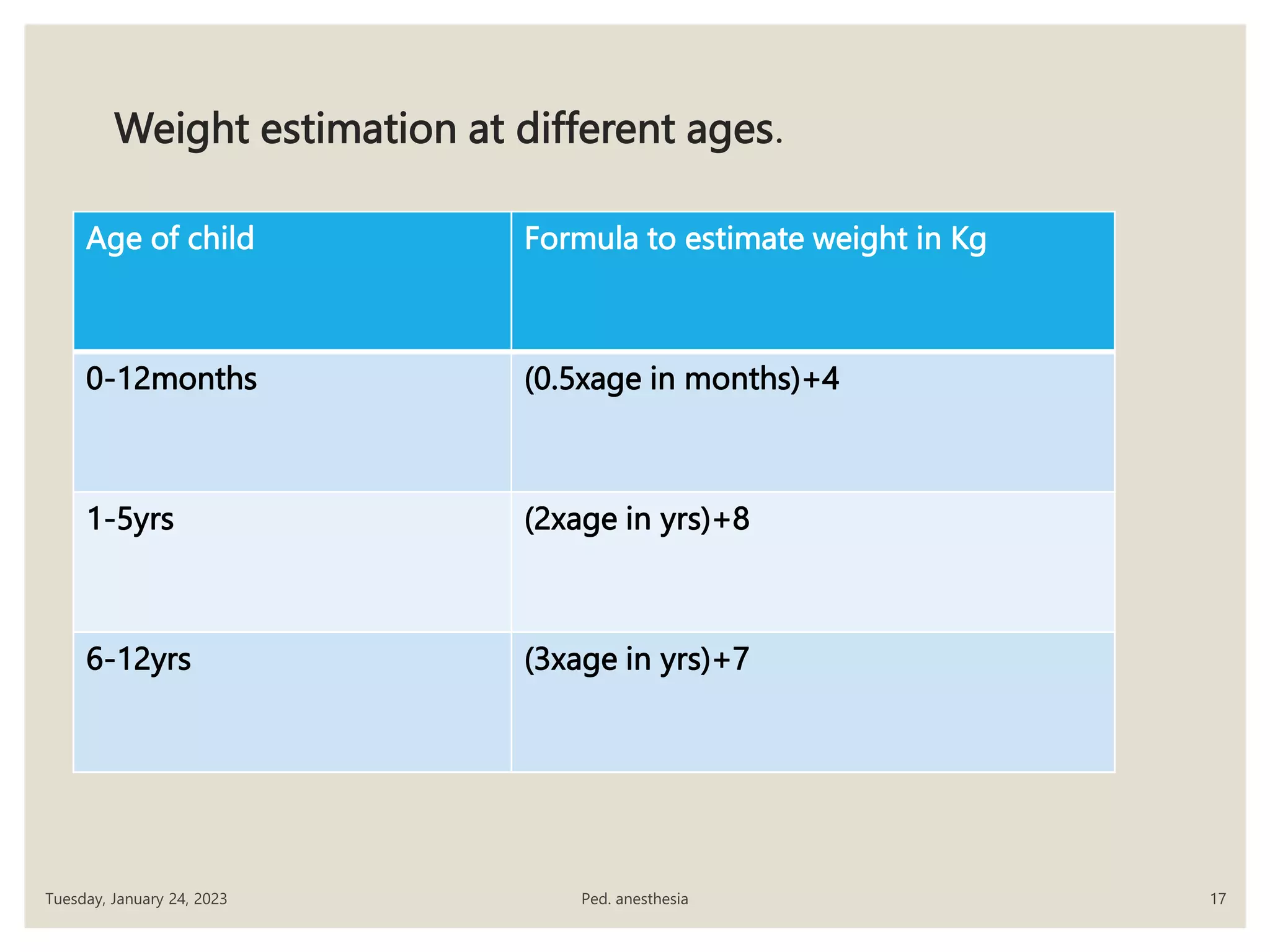
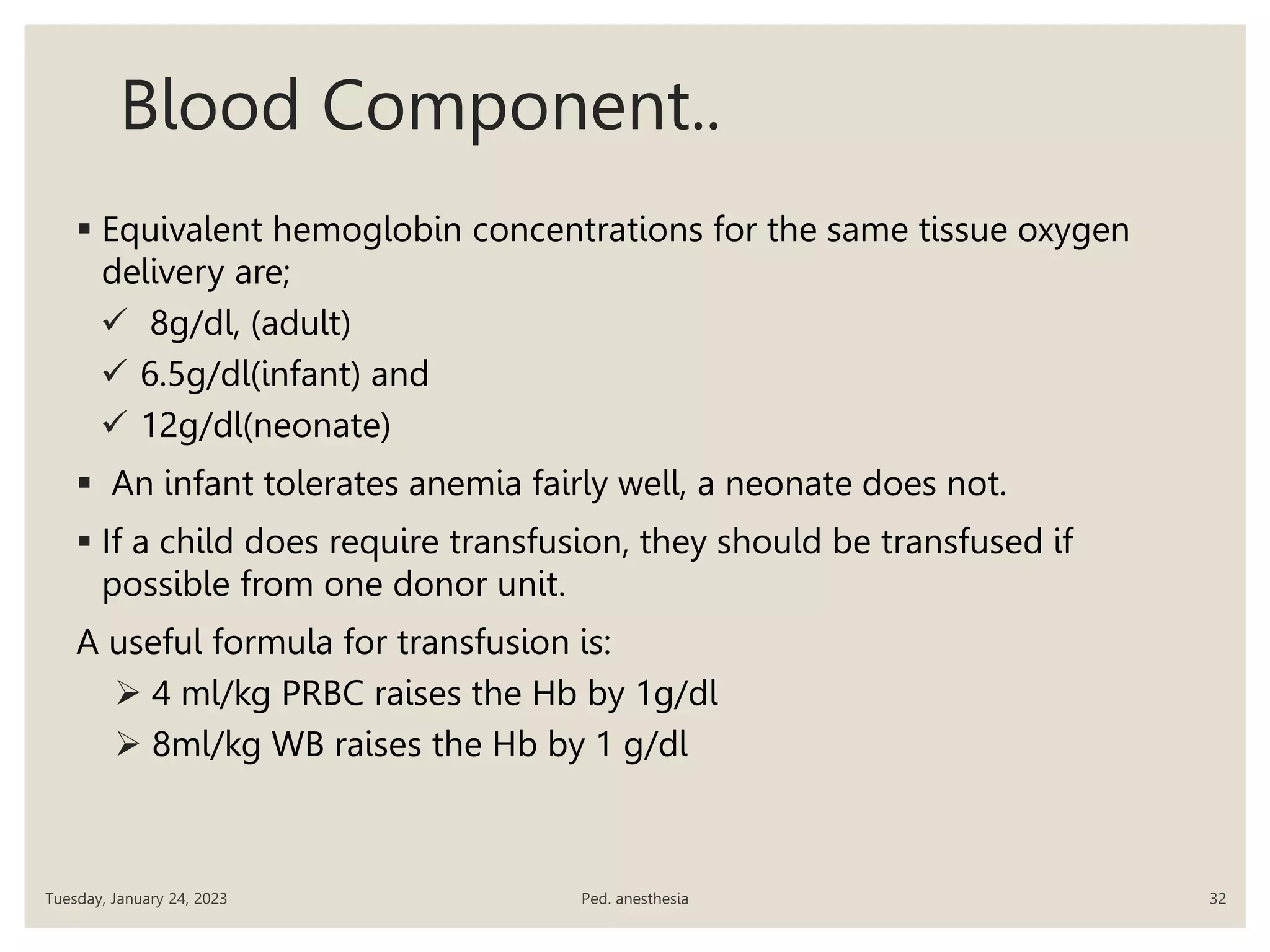
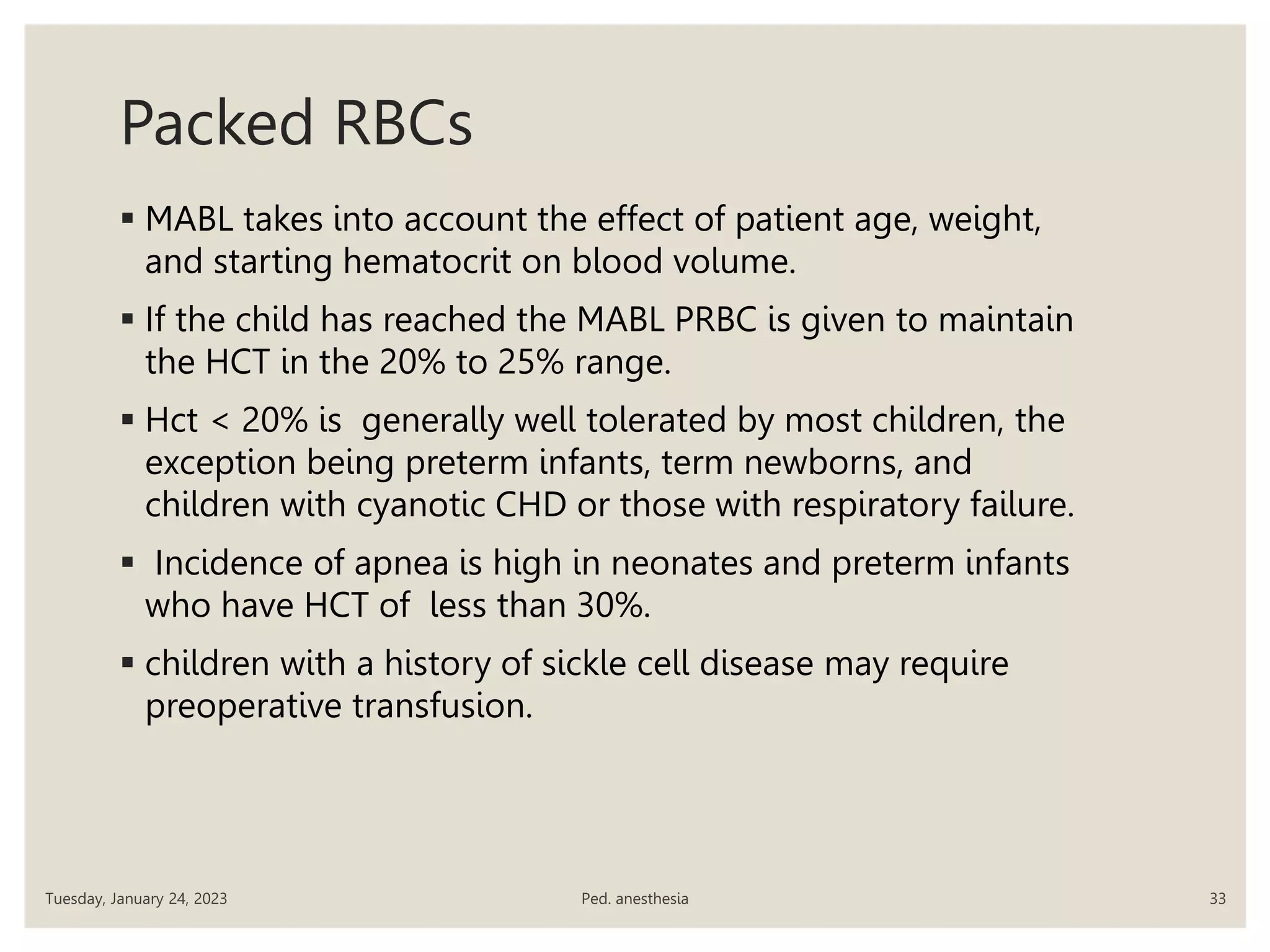
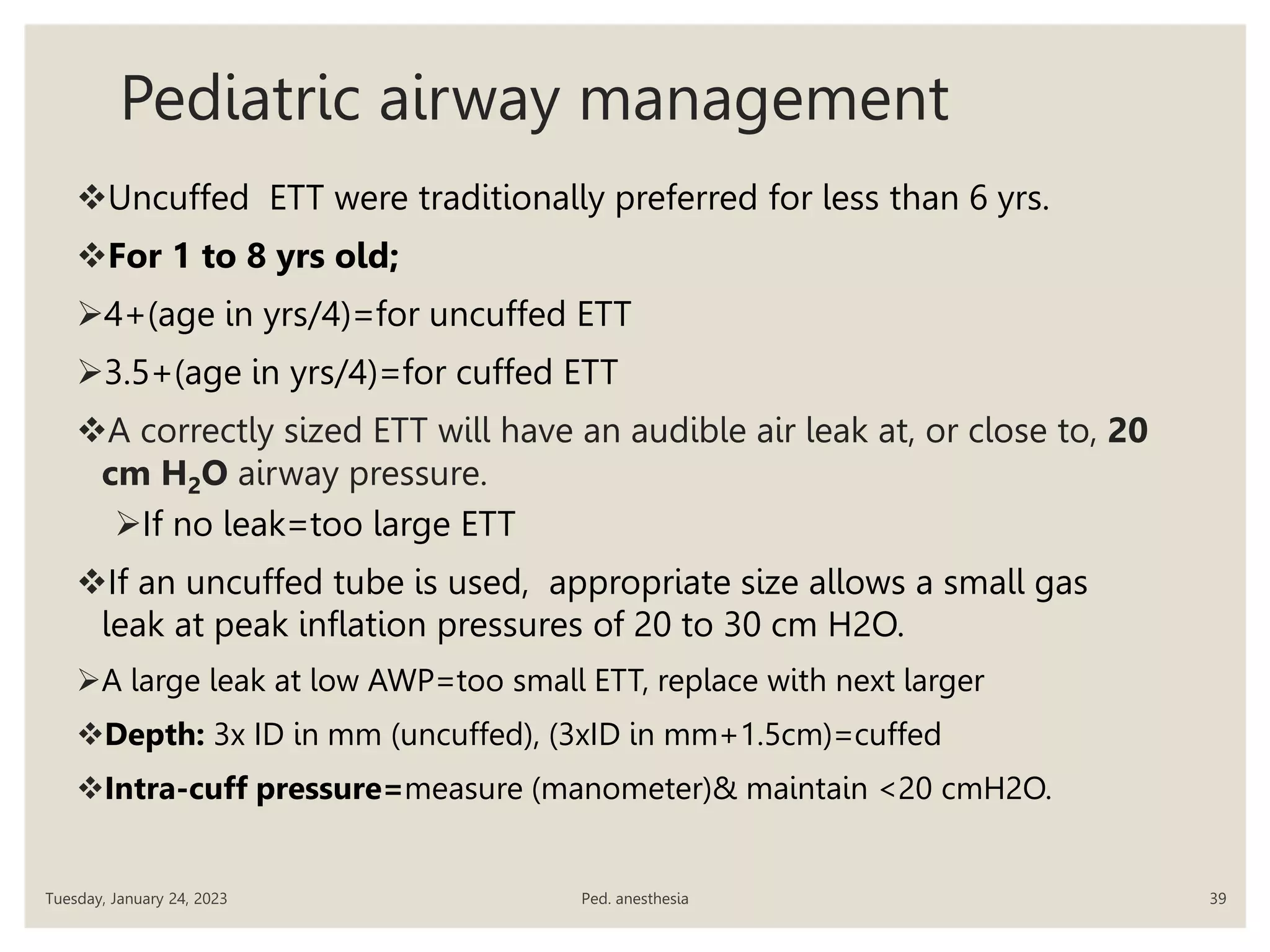
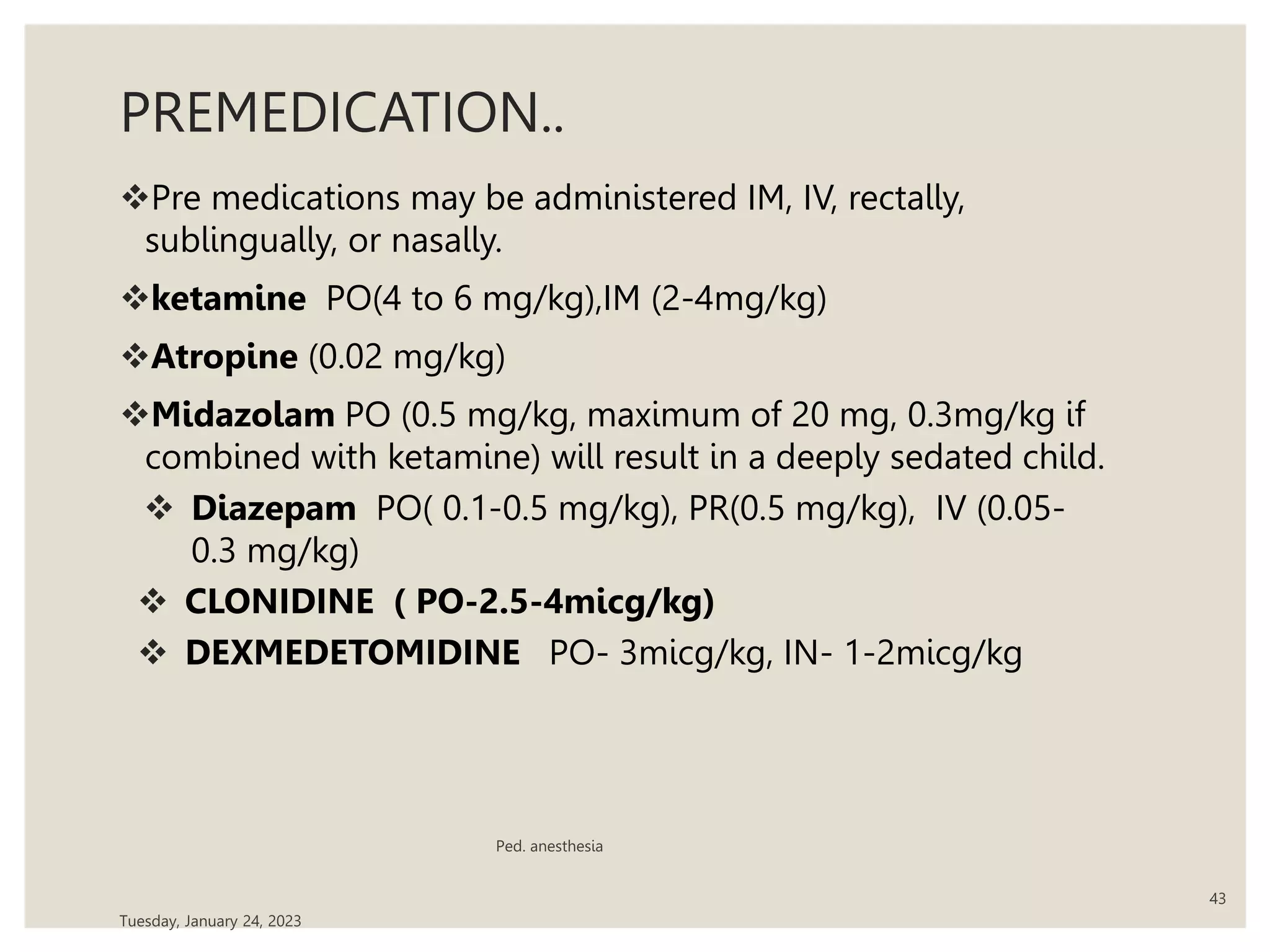
This document outlines a presentation on pediatric anesthesia. It discusses the anatomical, physiological, and pharmacological differences between pediatric patients and adults that are important for anesthesiologists to consider. Specifically, it notes that pediatric patients have higher heart rates, metabolic rates, and fluid volumes as a percentage of body weight compared to adults. The presentation also reviews preoperative evaluation and planning, fluid management, and techniques for airway management and induction of anesthesia in children. The overall objectives are for attendees to understand the unique concerns of pediatric anesthesia and to provide safe care for this patient population.