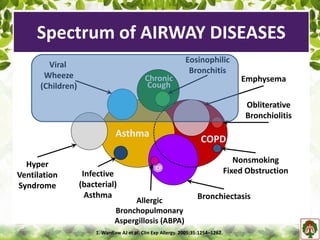
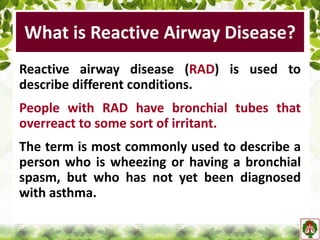
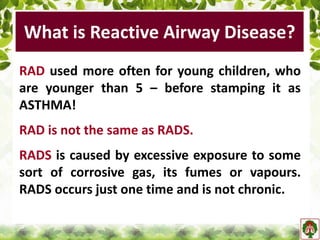
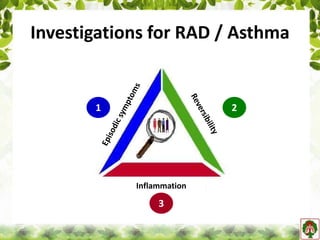
The document discusses reactive airway disease (RAD), describing it as a condition where bronchial tubes overreact to irritants, often seen in young children before a diagnosis of asthma is made. It outlines clinical presentations, diagnostic methods, and management strategies for RAD and other related conditions such as asthma and COPD, emphasizing the importance of airflow limitation and inflammation in diagnosis. Additionally, it highlights different tests and assessments used to monitor and diagnose airway diseases.