This document discusses various nerve blocks for thoracic and abdominal pain management including:
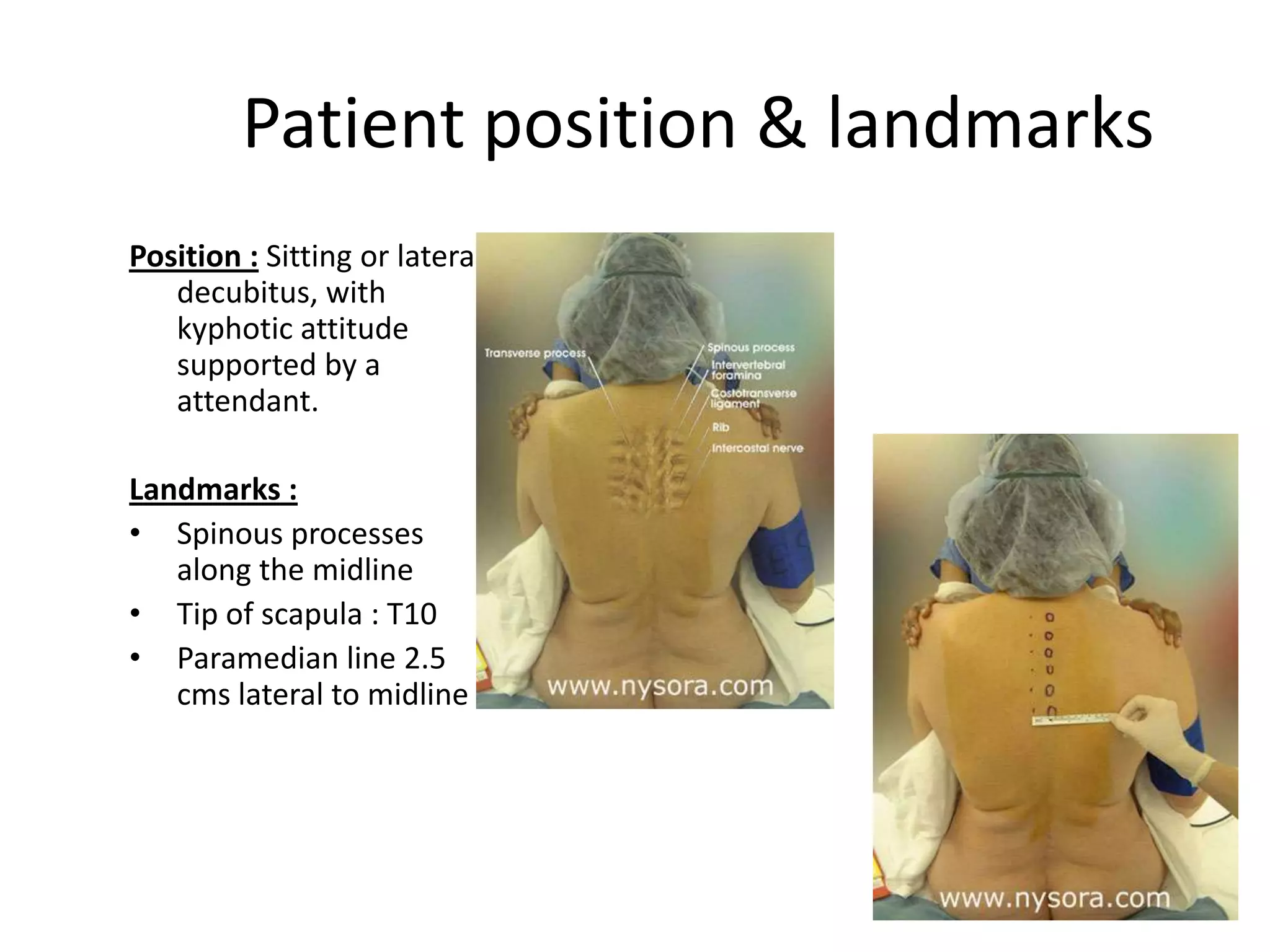
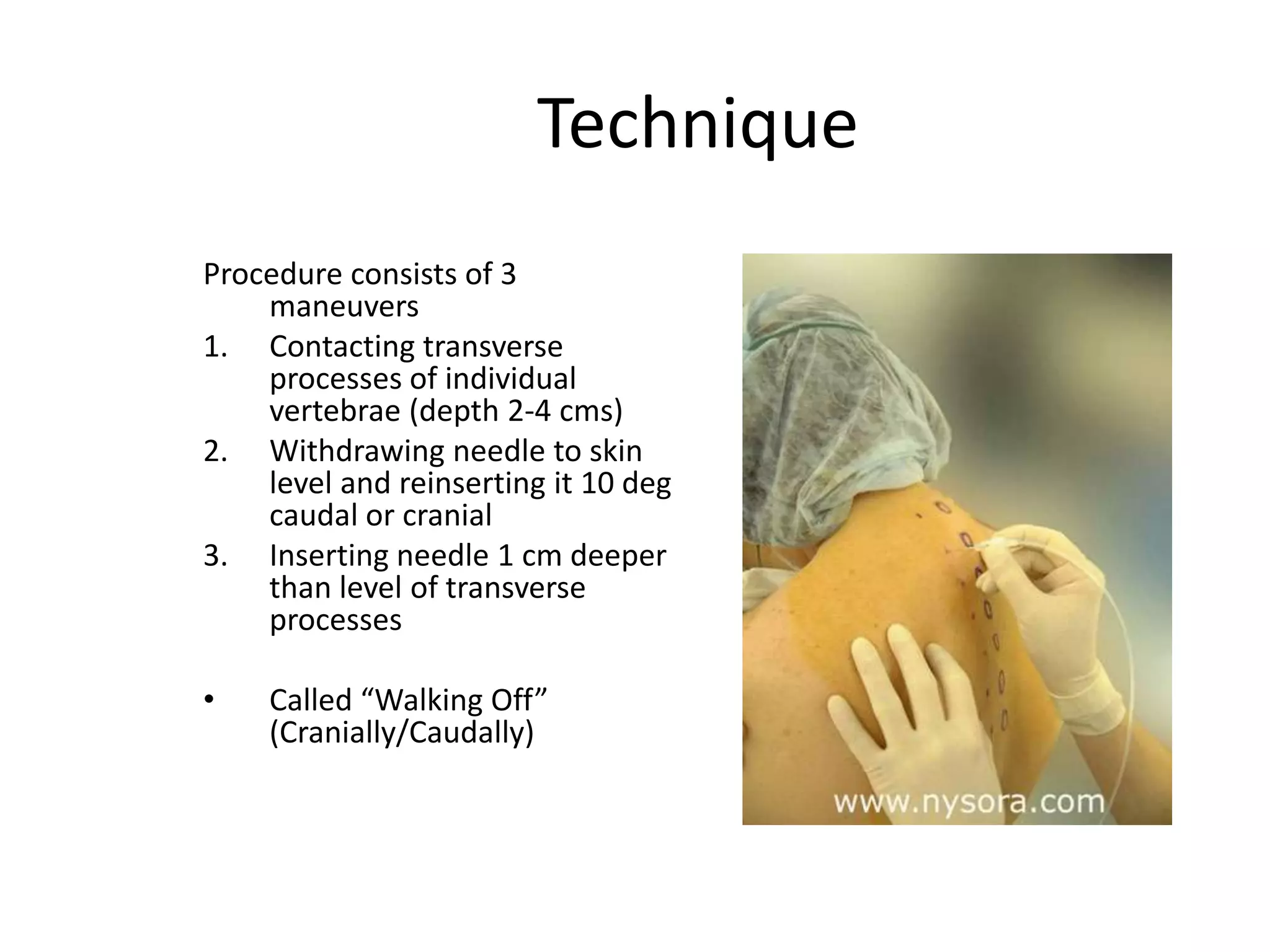
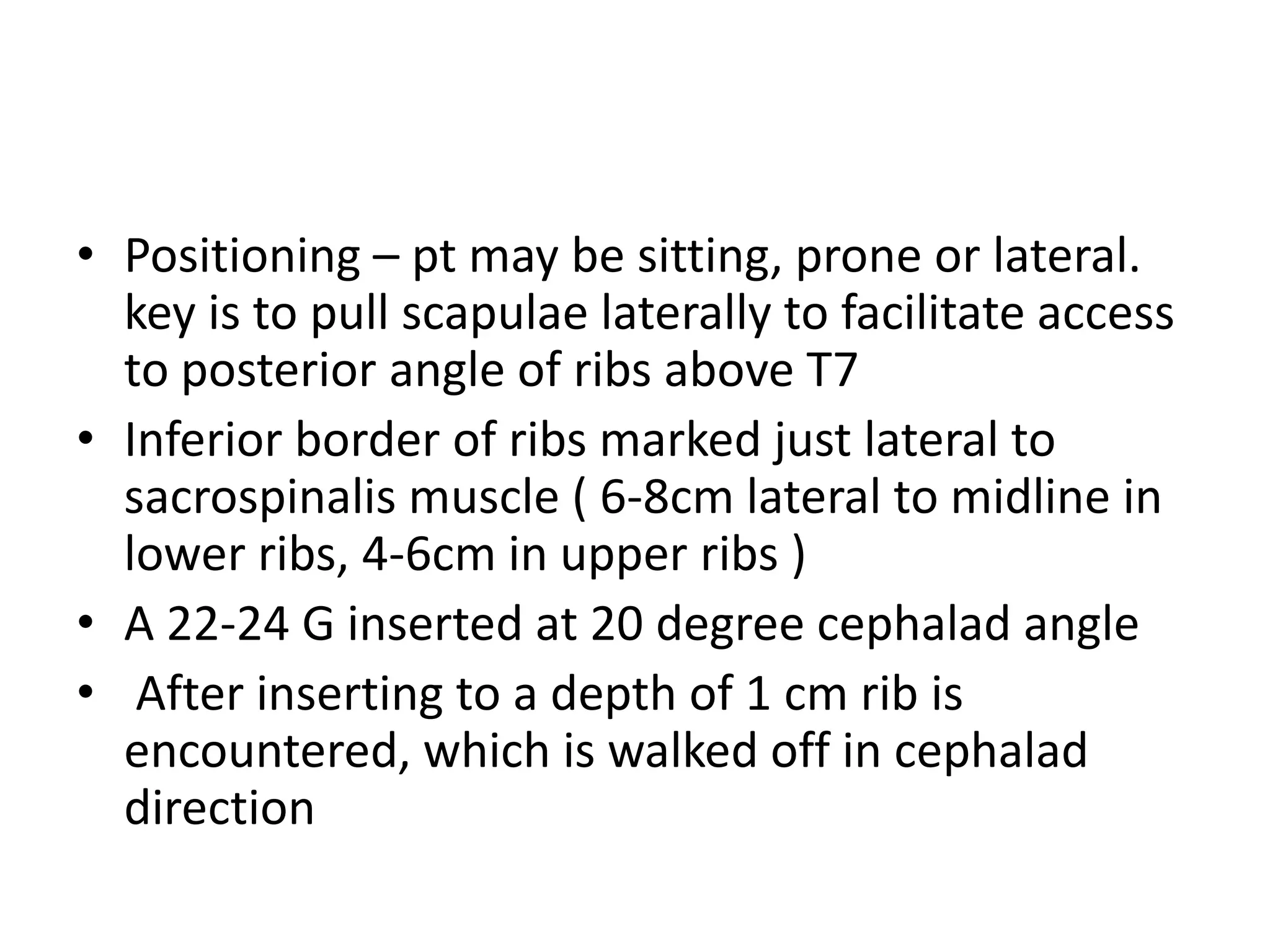
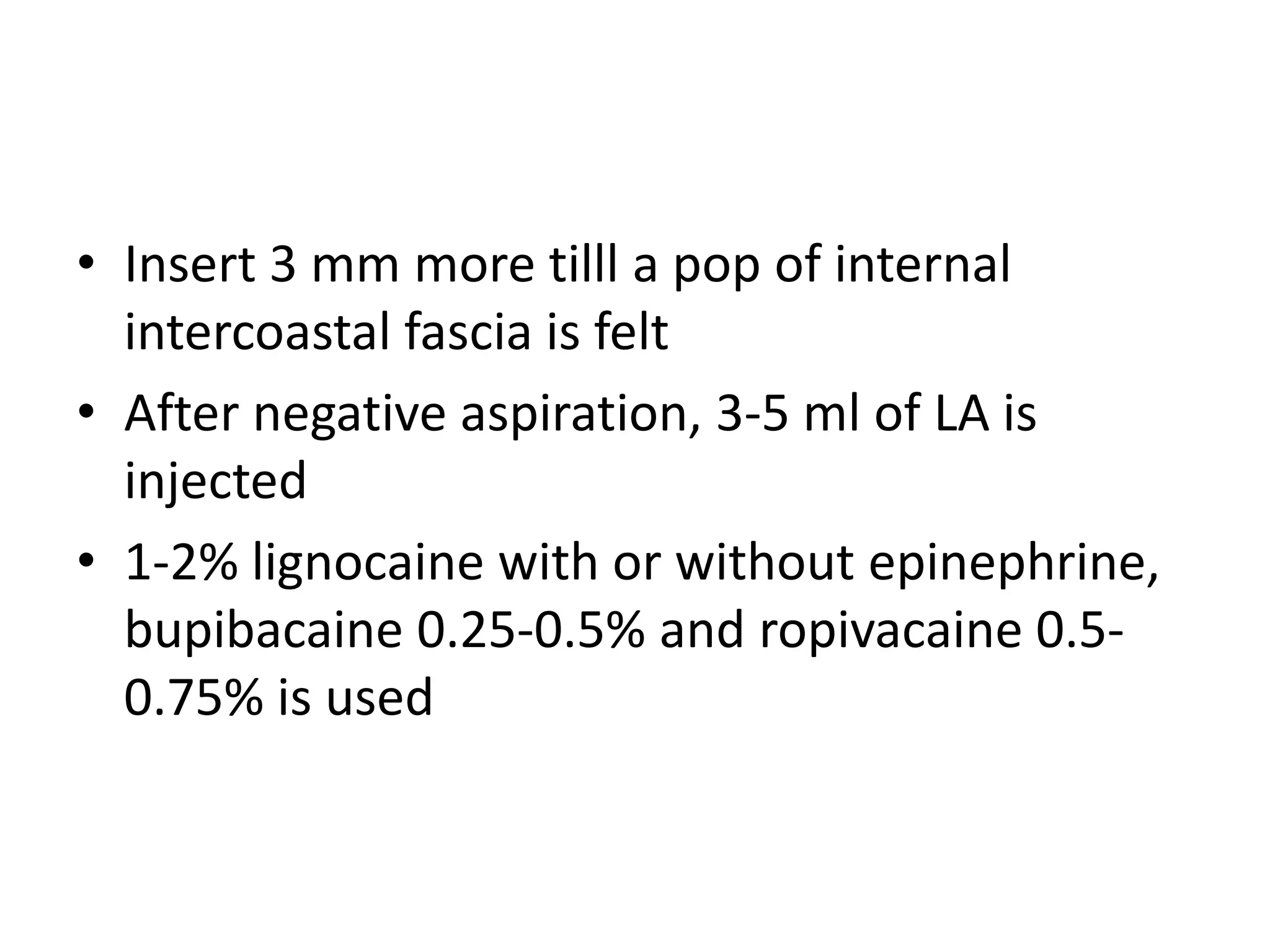
1. Paravertebral blocks are commonly used for postoperative analgesia after thoracic and breast surgeries as well as for rib fractures and herpes zoster pain.
2. Intercostal nerve blocks provide analgesia after procedures like thoracotomy but are rarely adequate for intraoperative anesthesia.
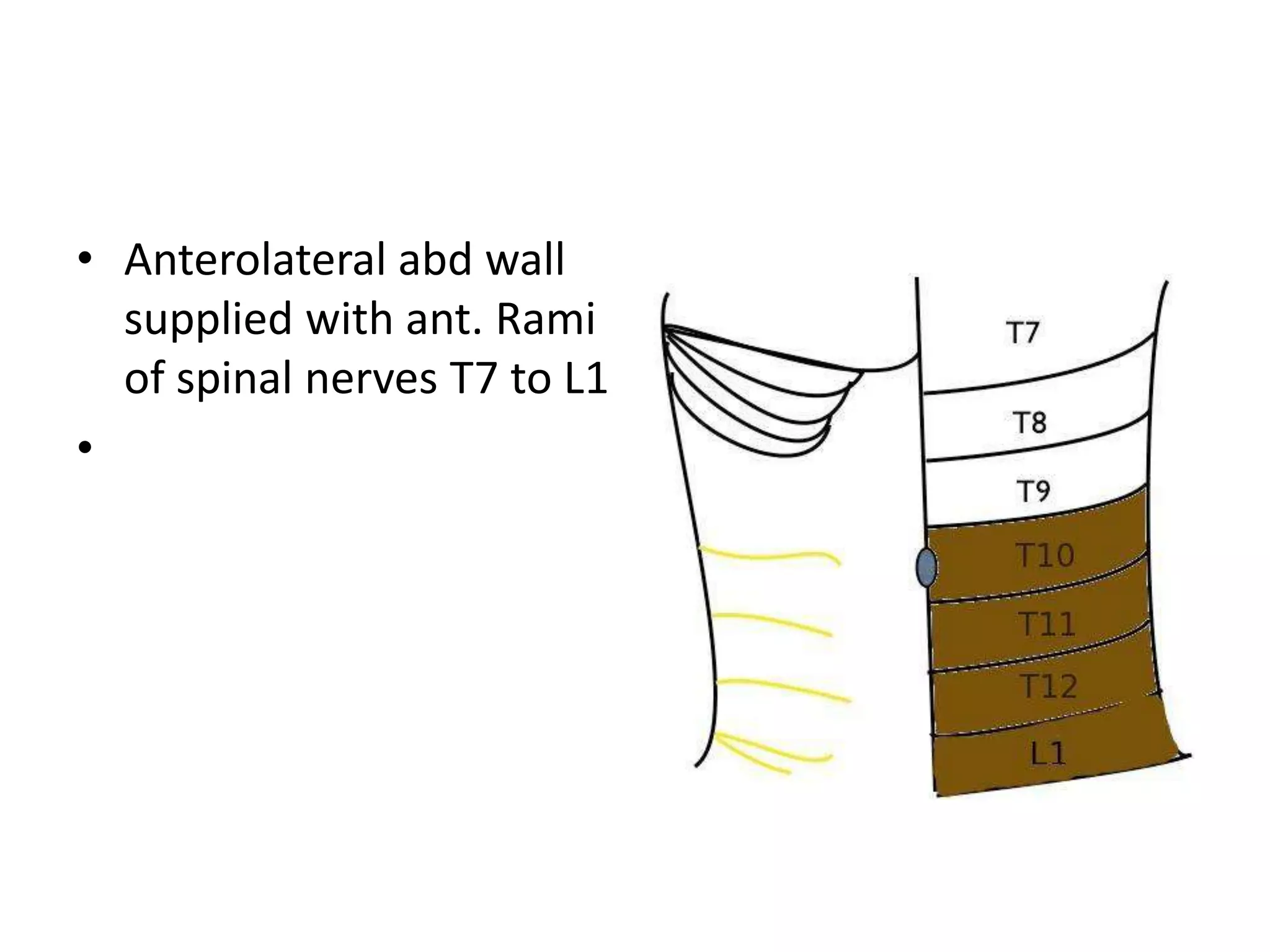
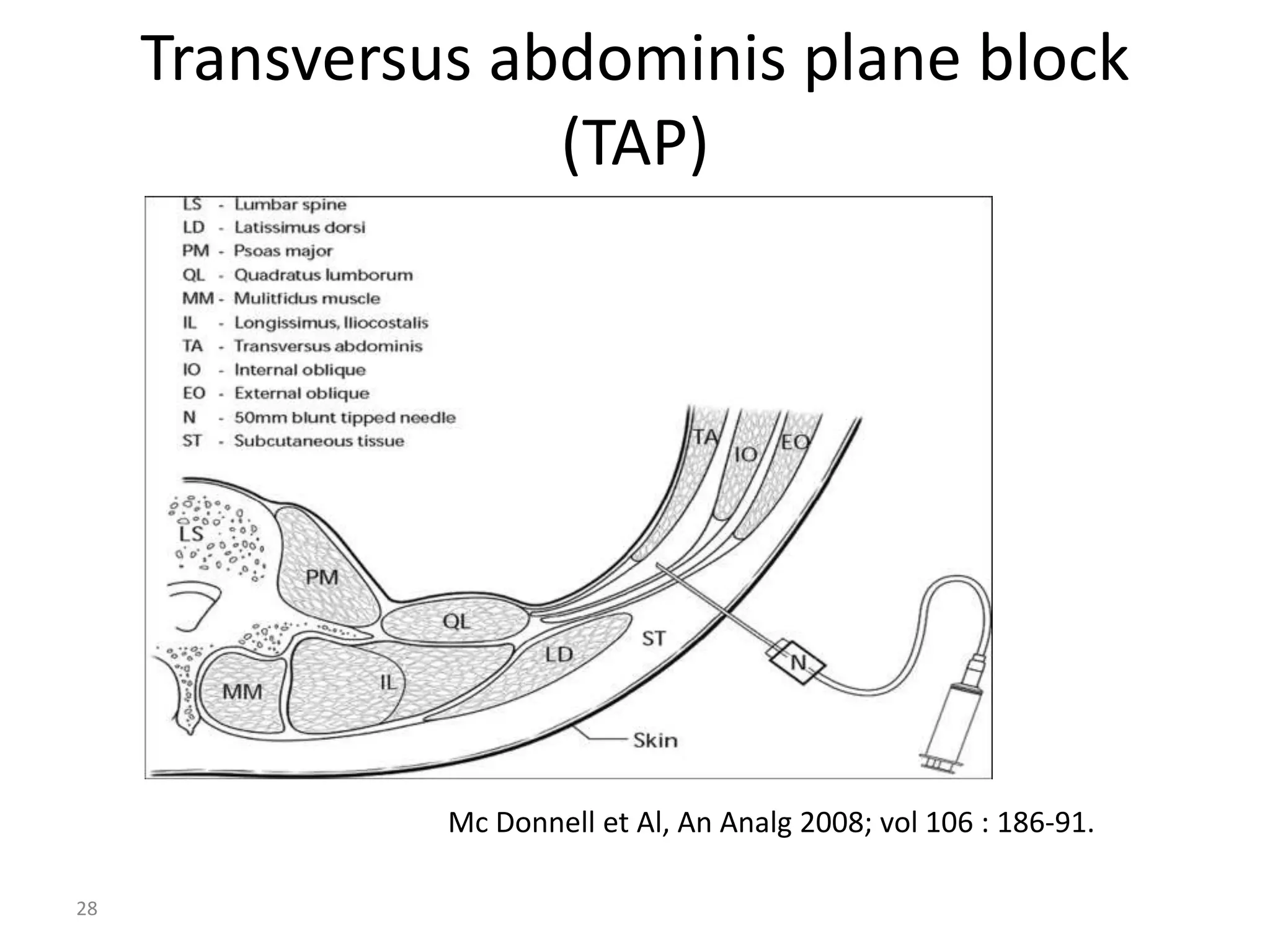
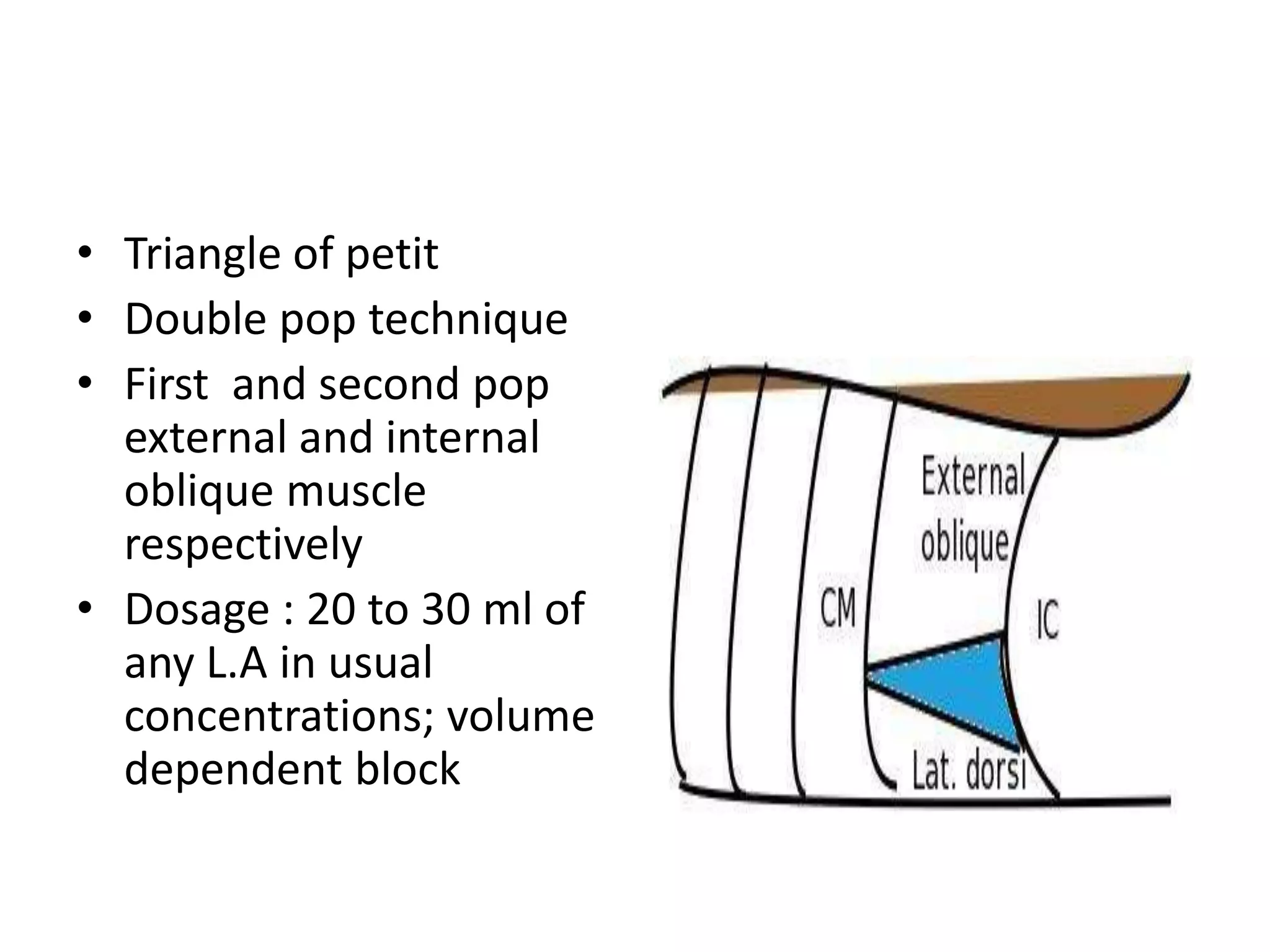
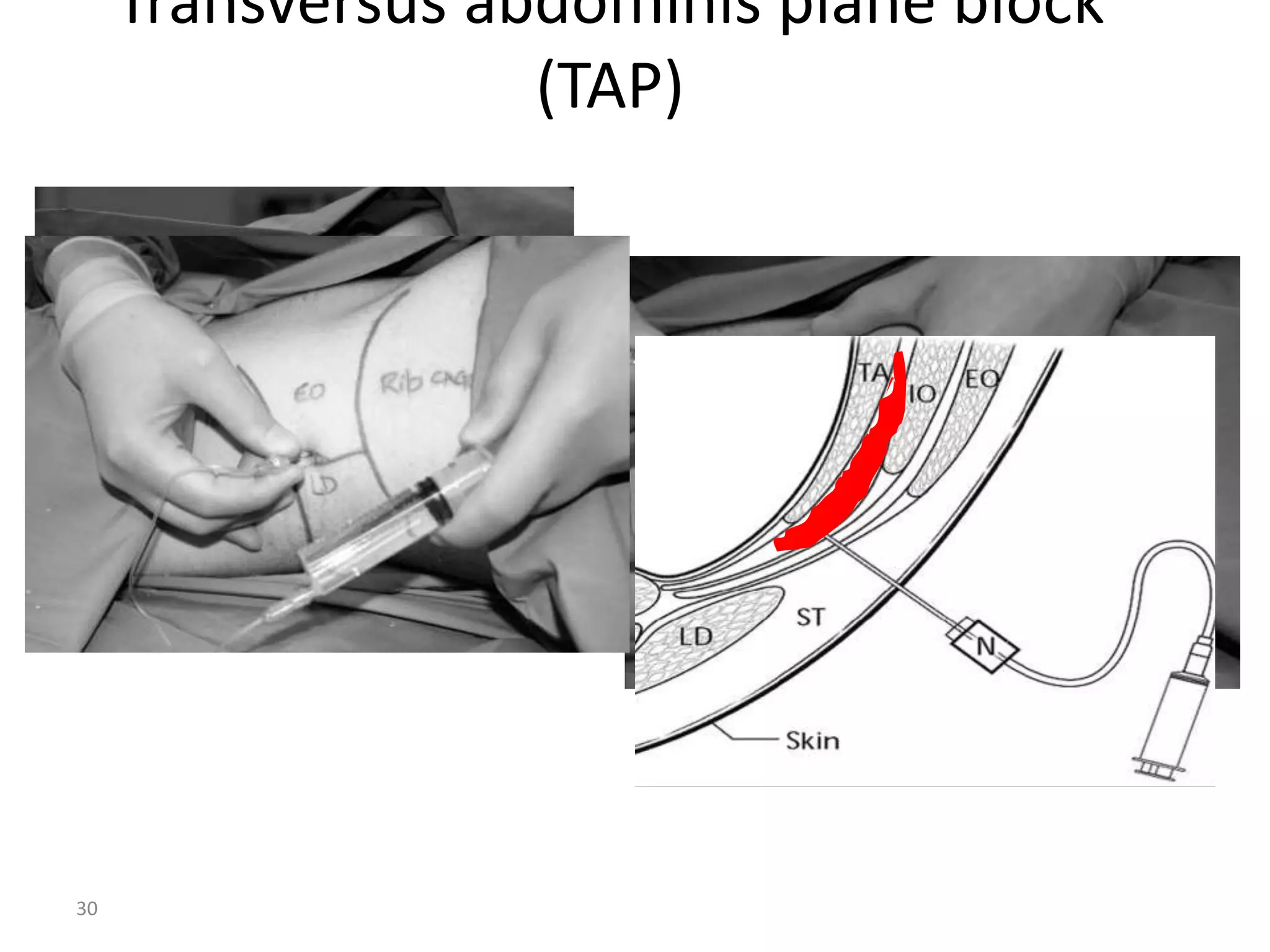
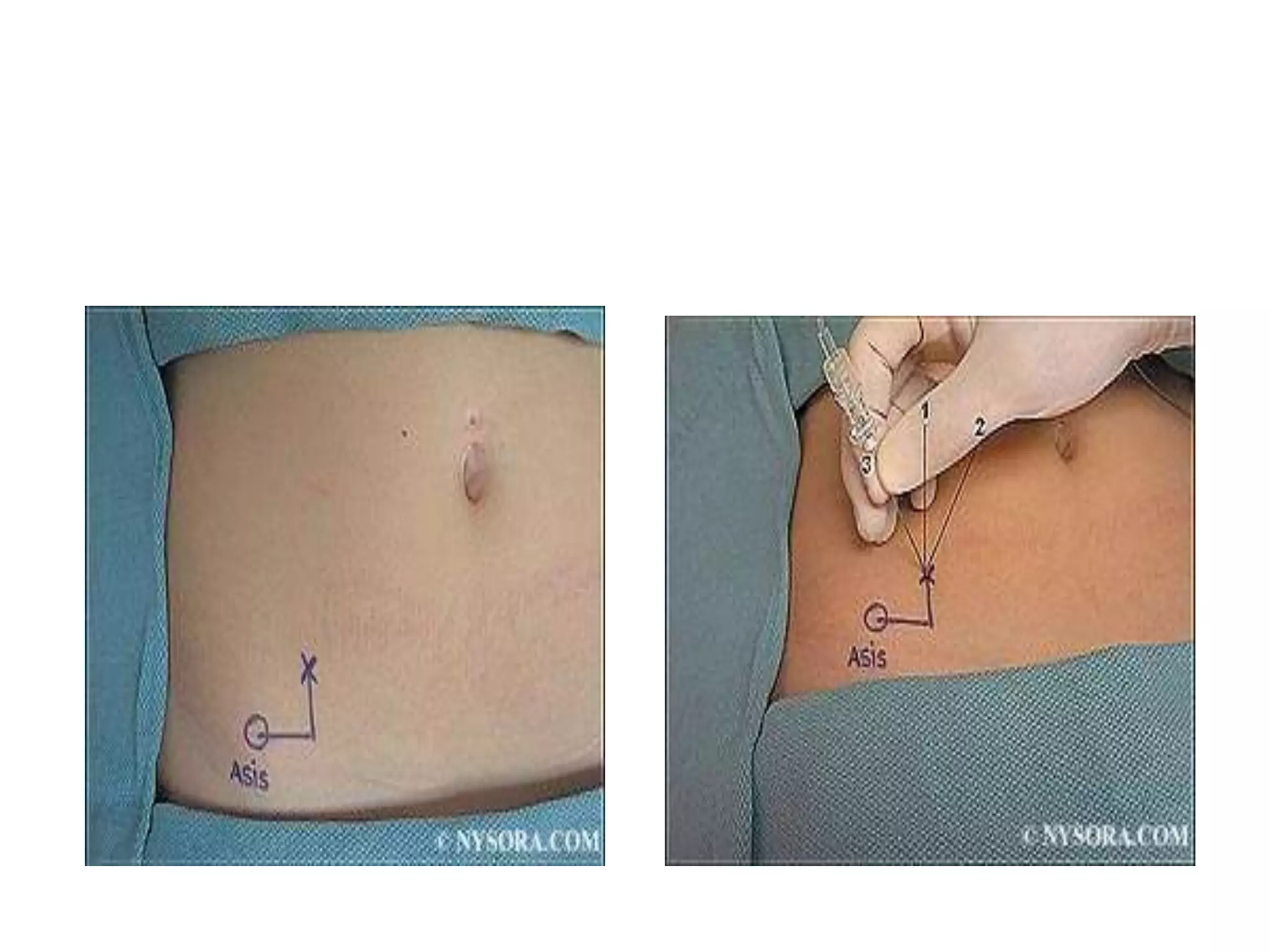
3. Transversus abdominis plane blocks are indicated for abdominal surgeries like appendectomy and hernia repair through the triangle of Petit technique.
4. Other blocks discussed include intrapleural, illioinguinal, illiohypogastric, thoracic epidural, and c