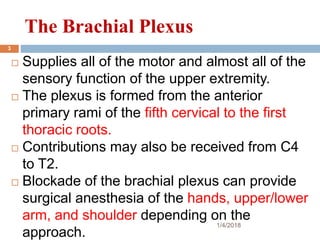
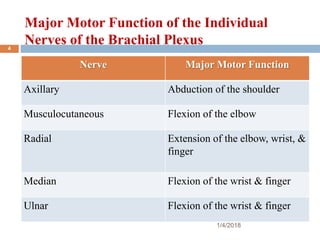
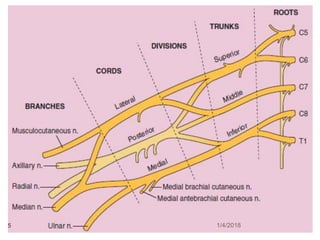
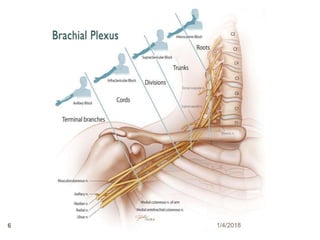
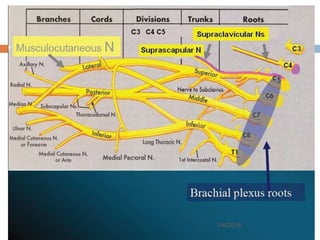
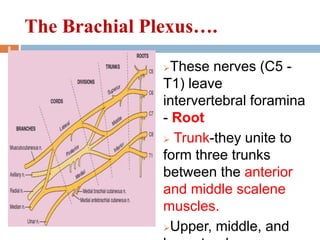
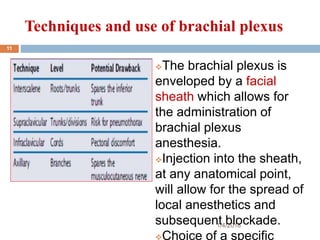
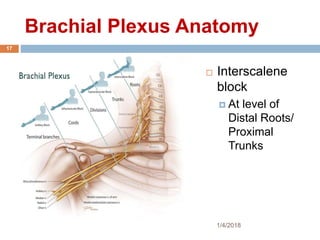
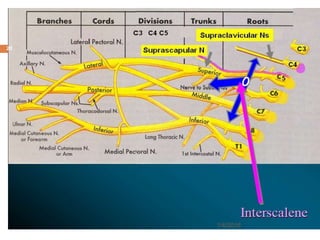
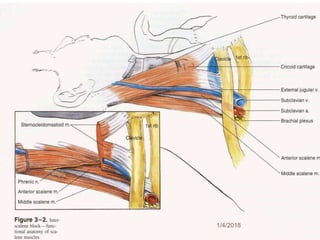
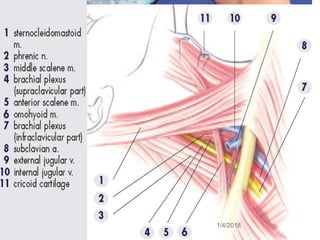
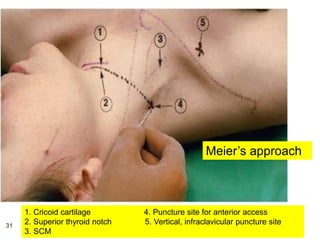
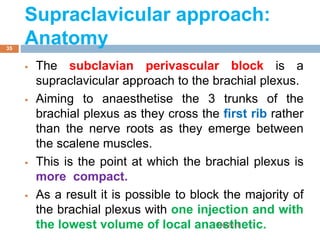
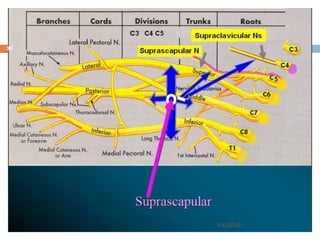
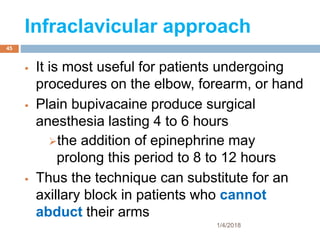
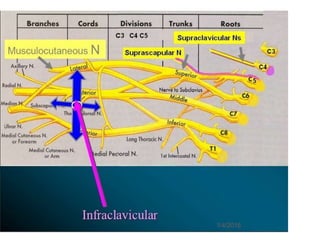
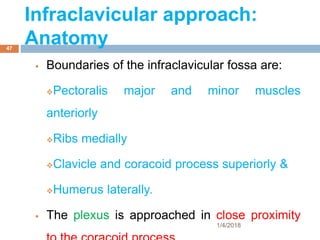
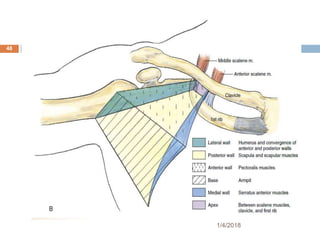
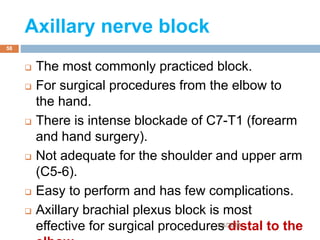
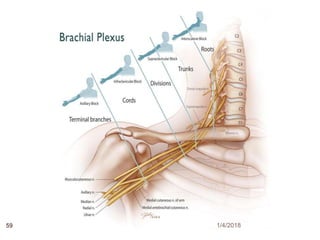
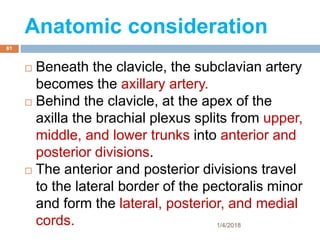
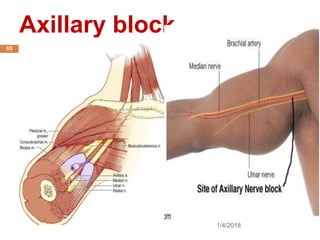
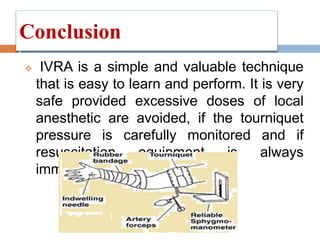
1) The document outlines different techniques for blocking the brachial plexus including interscalene, supraclavicular, infraclavicular, and axillary approaches.
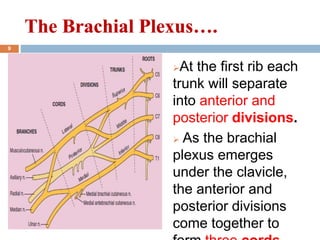
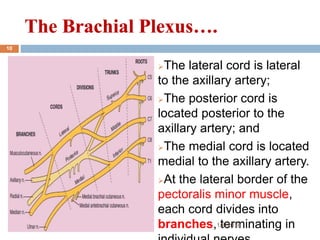
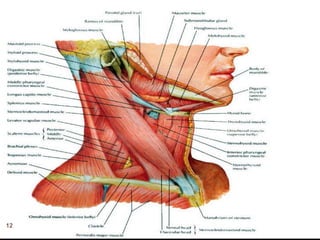
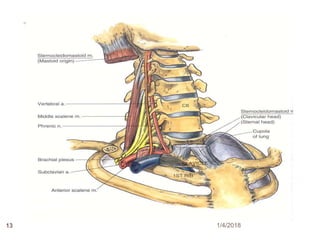
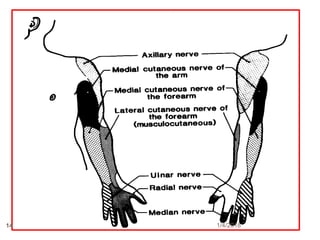
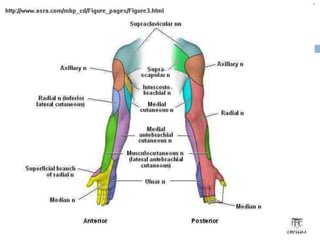
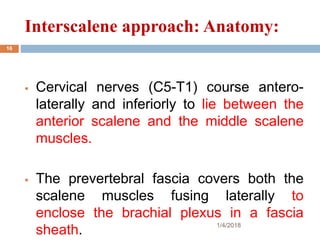
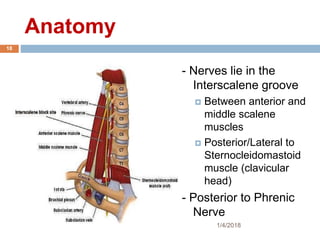
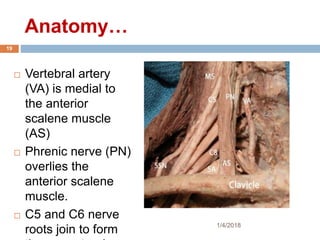
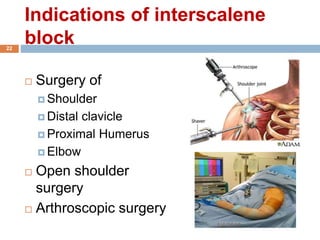
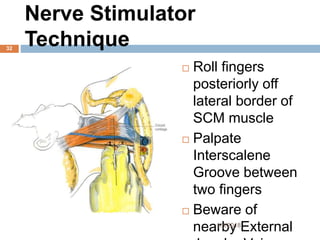
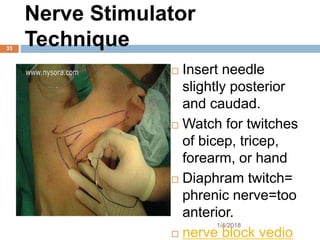
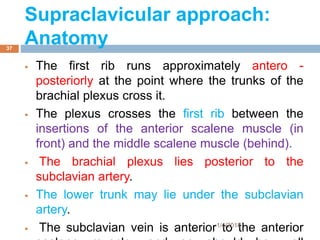
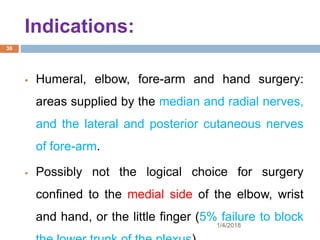
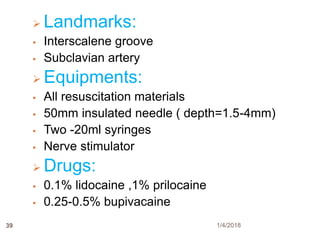
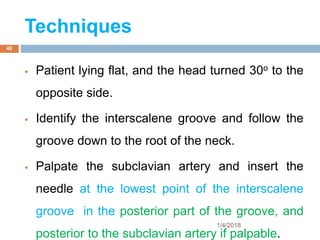
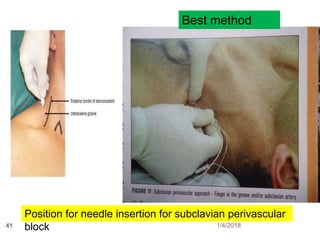
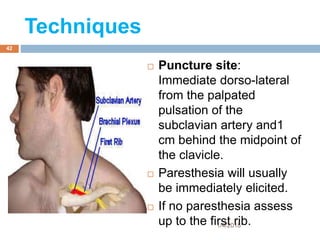
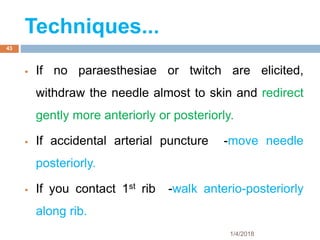
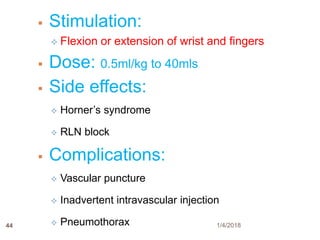
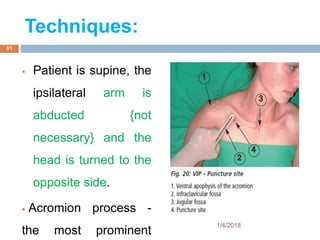
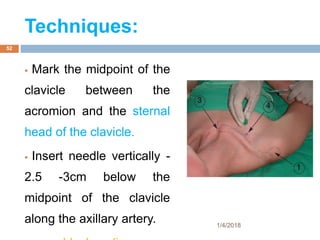
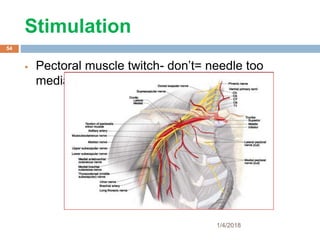
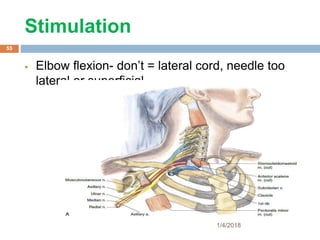
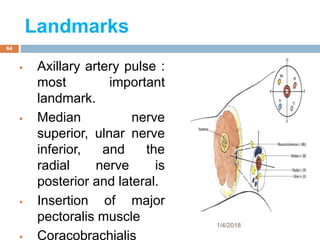
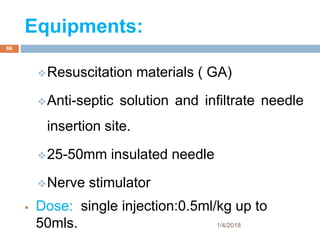
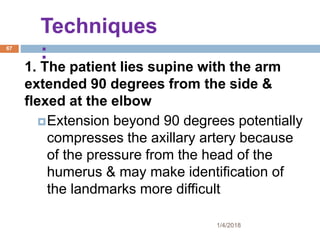
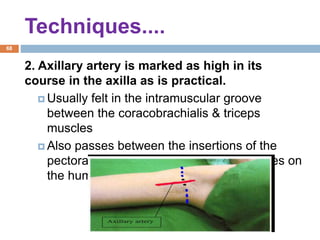
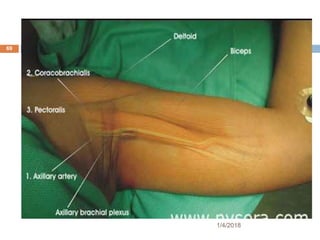
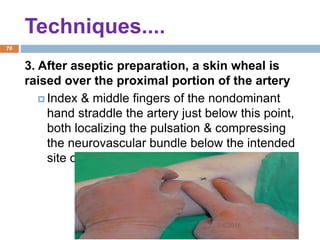
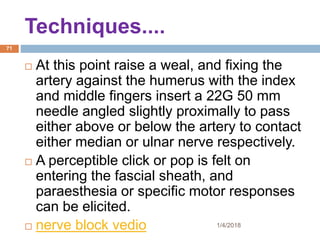
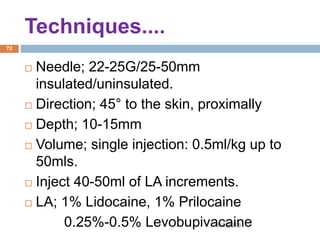
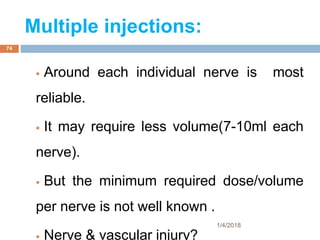
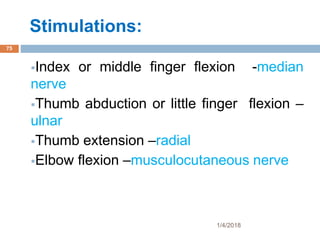
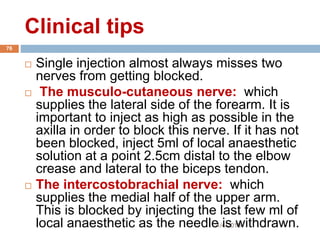
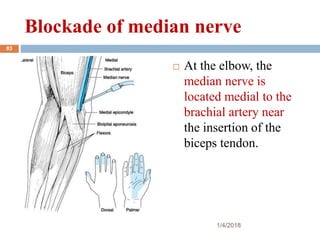
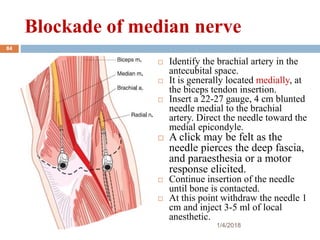
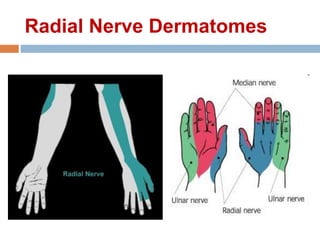
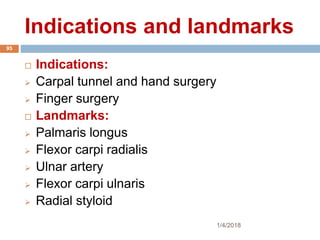
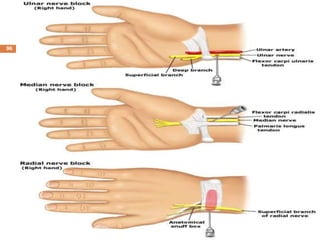
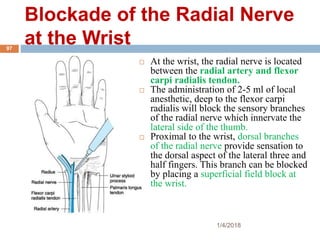
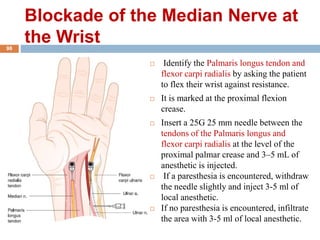
2) Each approach is described in terms of relevant anatomy, indications, landmarks, equipment, drugs, and techniques.
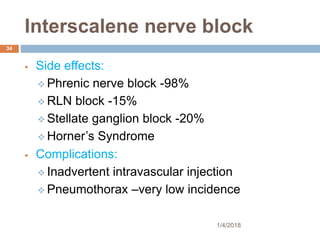
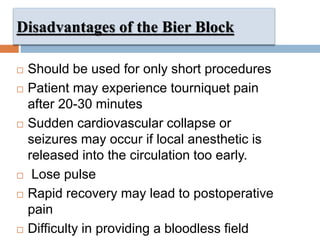
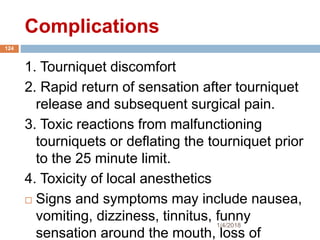
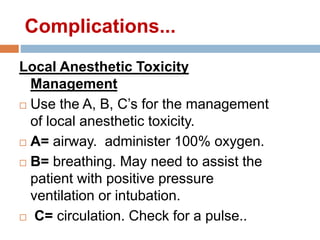
3) Potential side effects and complications are also reviewed such as phrenic nerve block, Horner's syndrome, and pneumothorax.