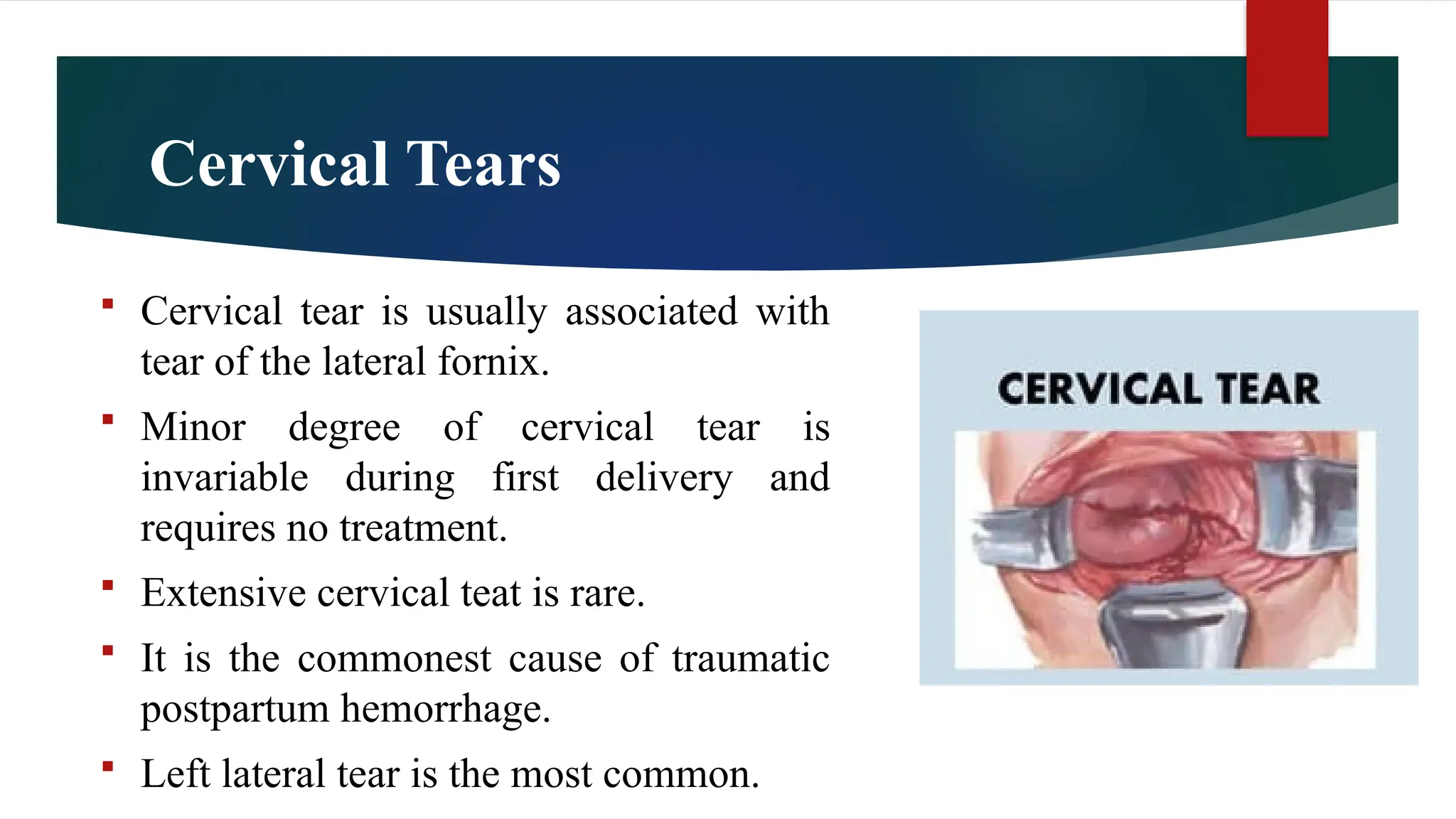
Injuries to the birth canal during childbirth are significant contributors to maternal morbidity and can occur in both natural and instrumental deliveries. Common types include perineal tears, cervical tears, and visceral injuries, each with specific causes, classifications, and management protocols. Effective prevention and timely repairs are crucial to minimizing long-term complications and ensuring maternal health.