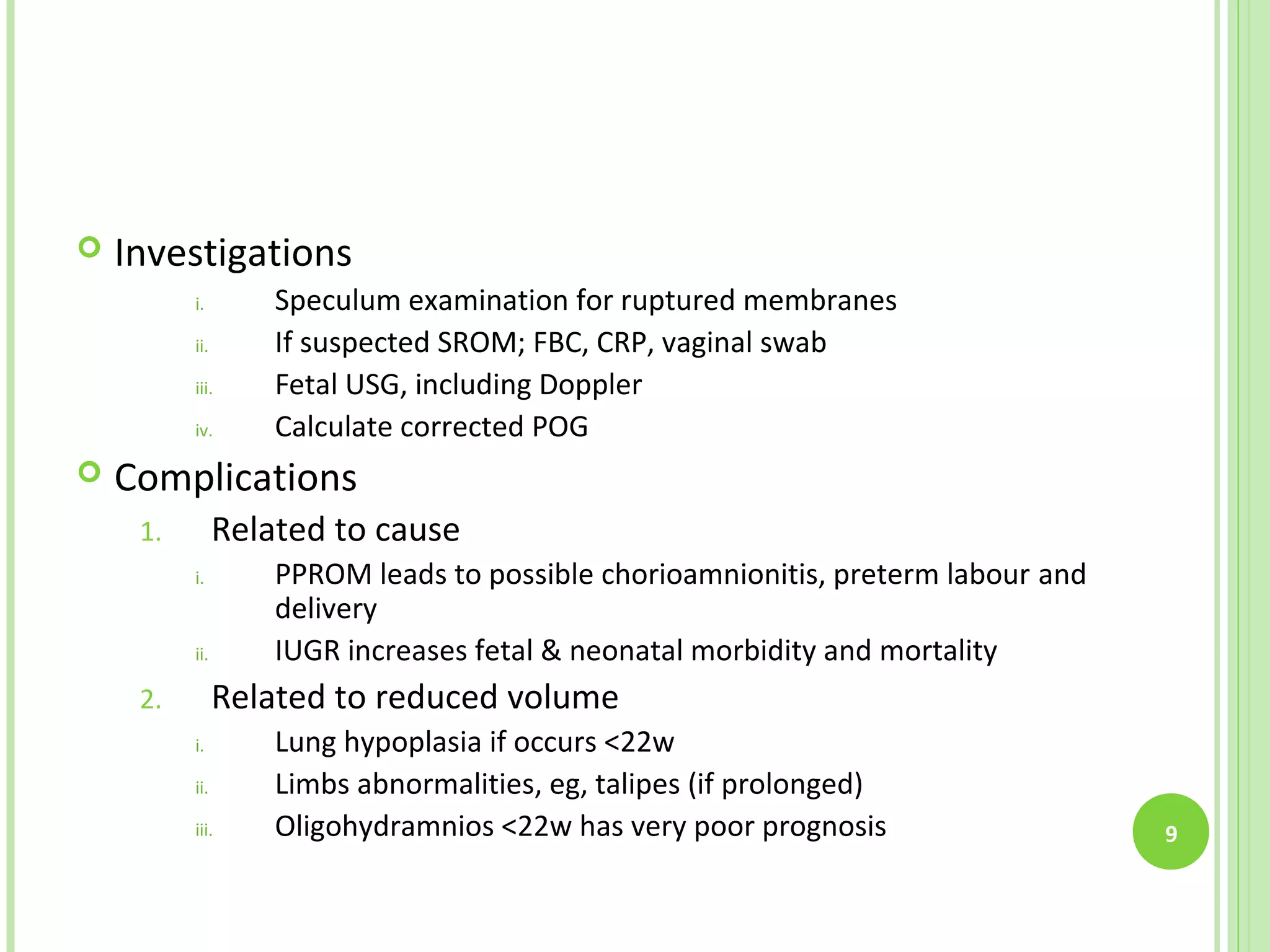
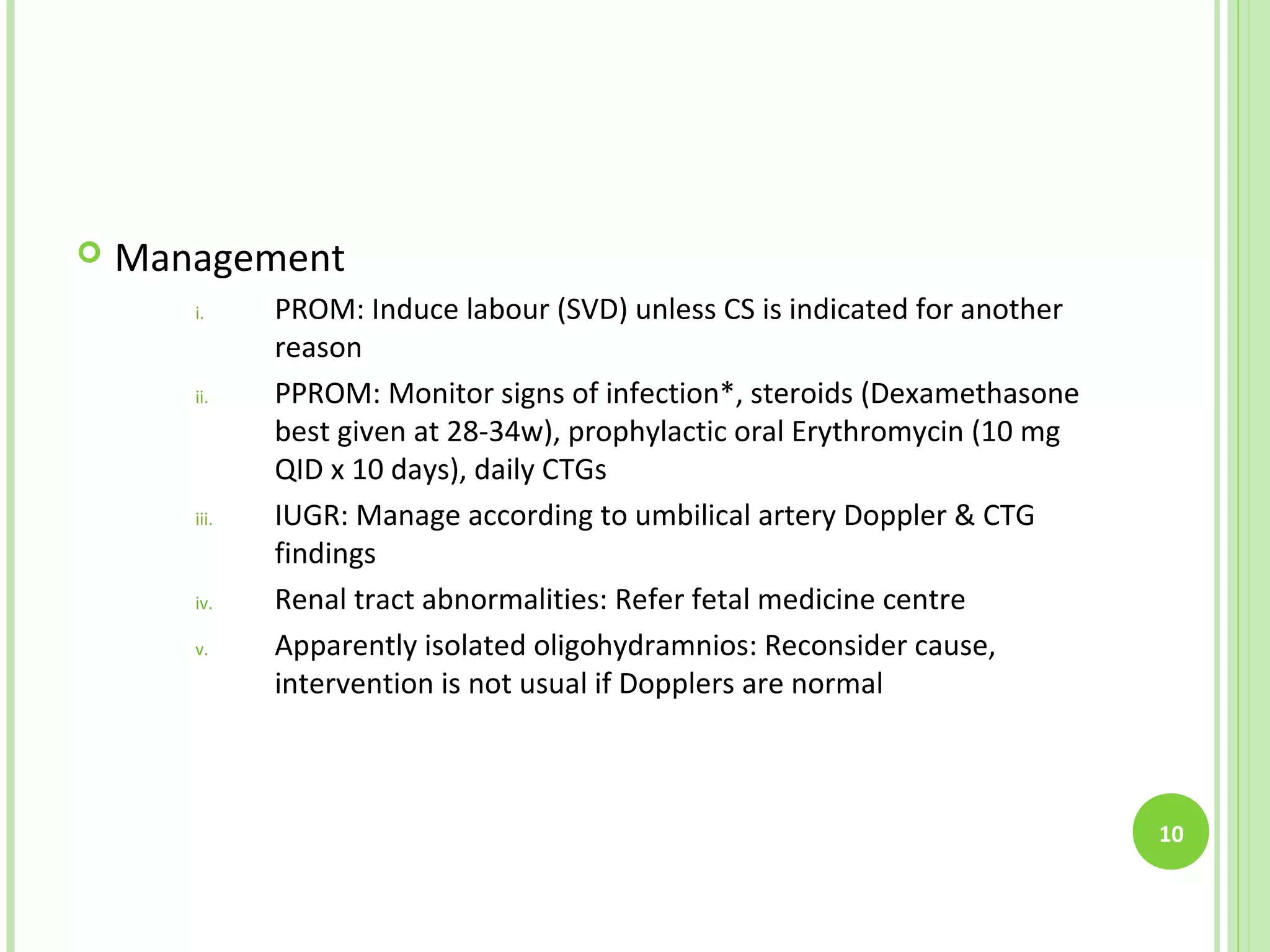
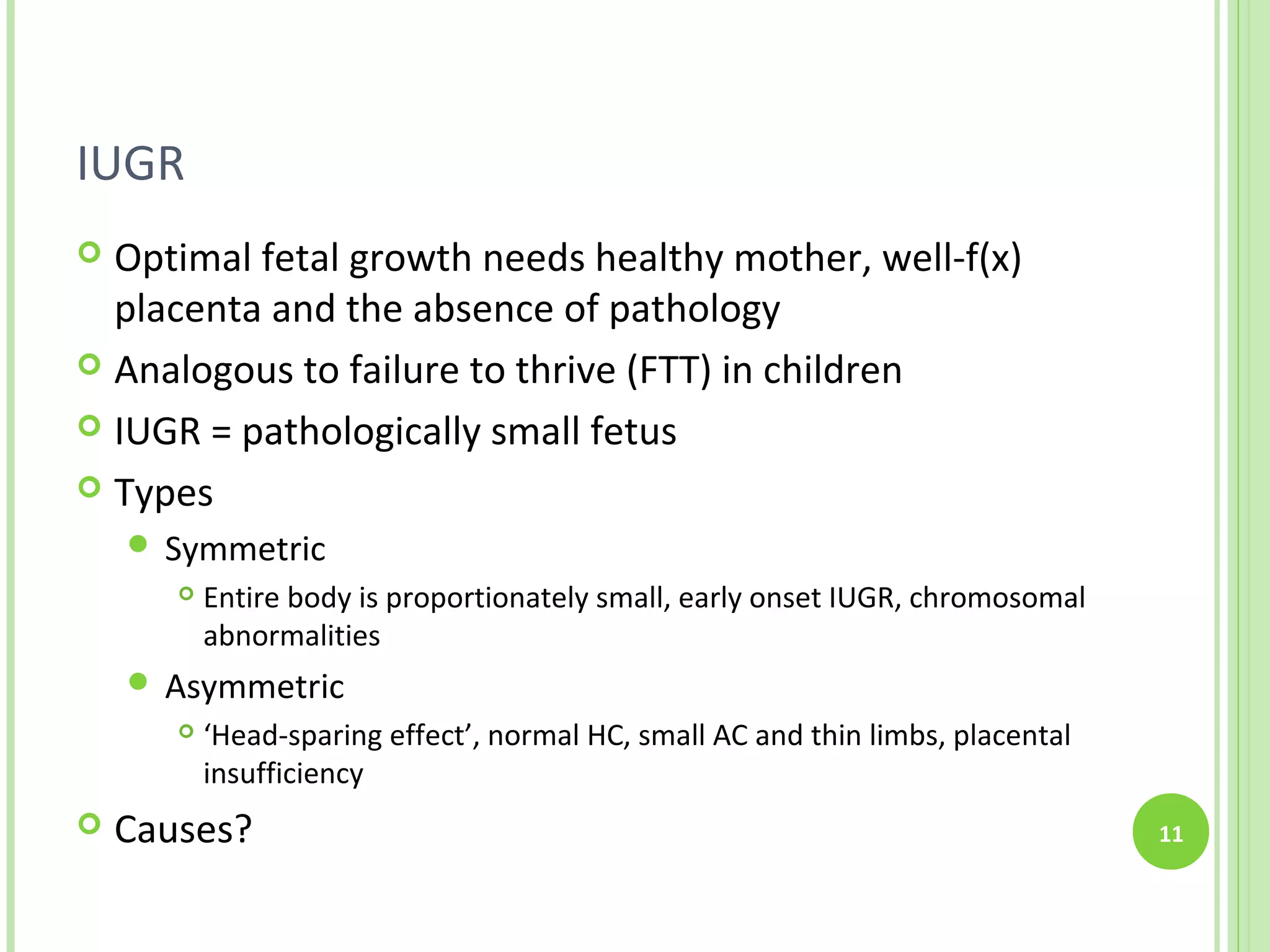
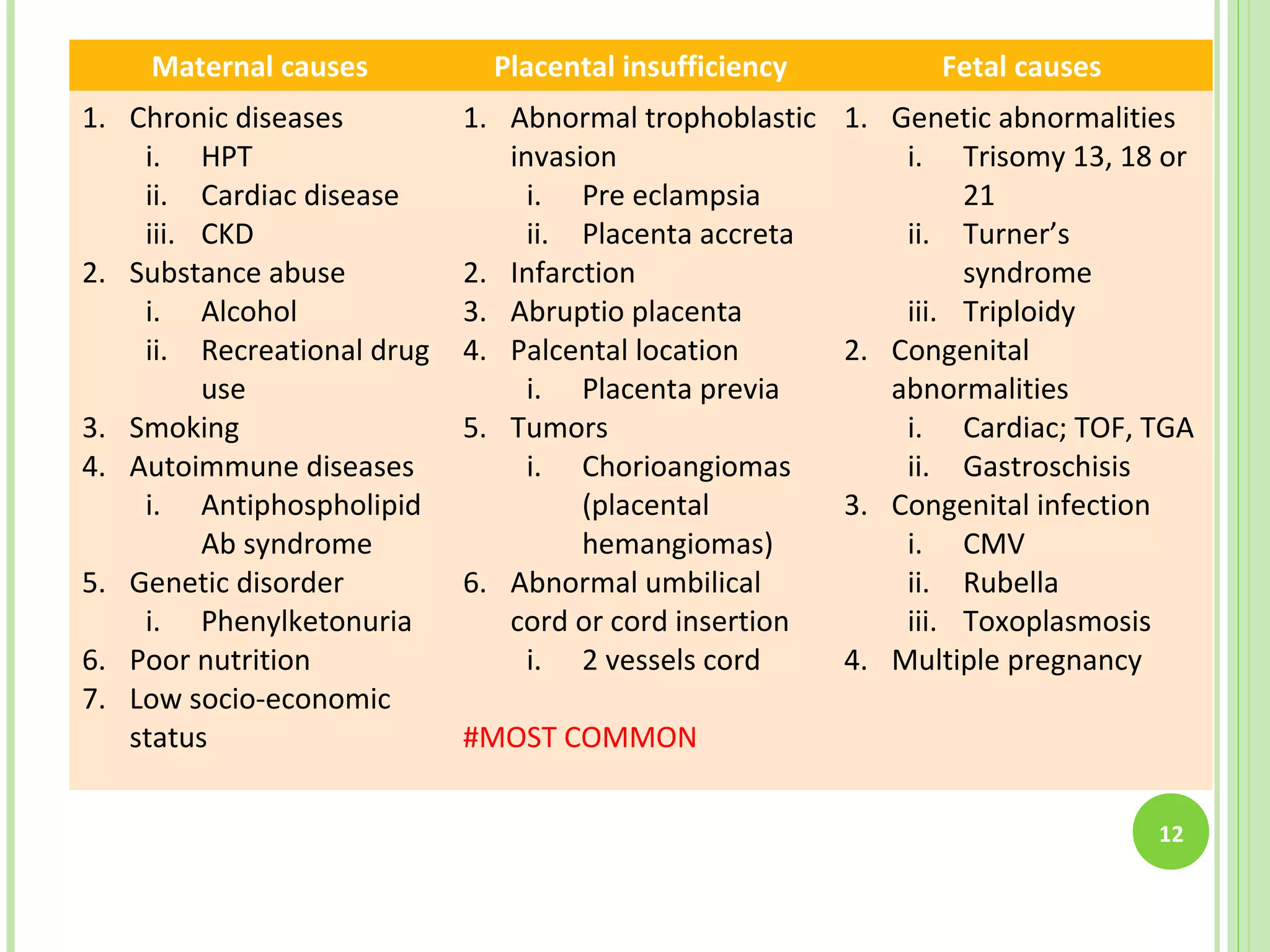
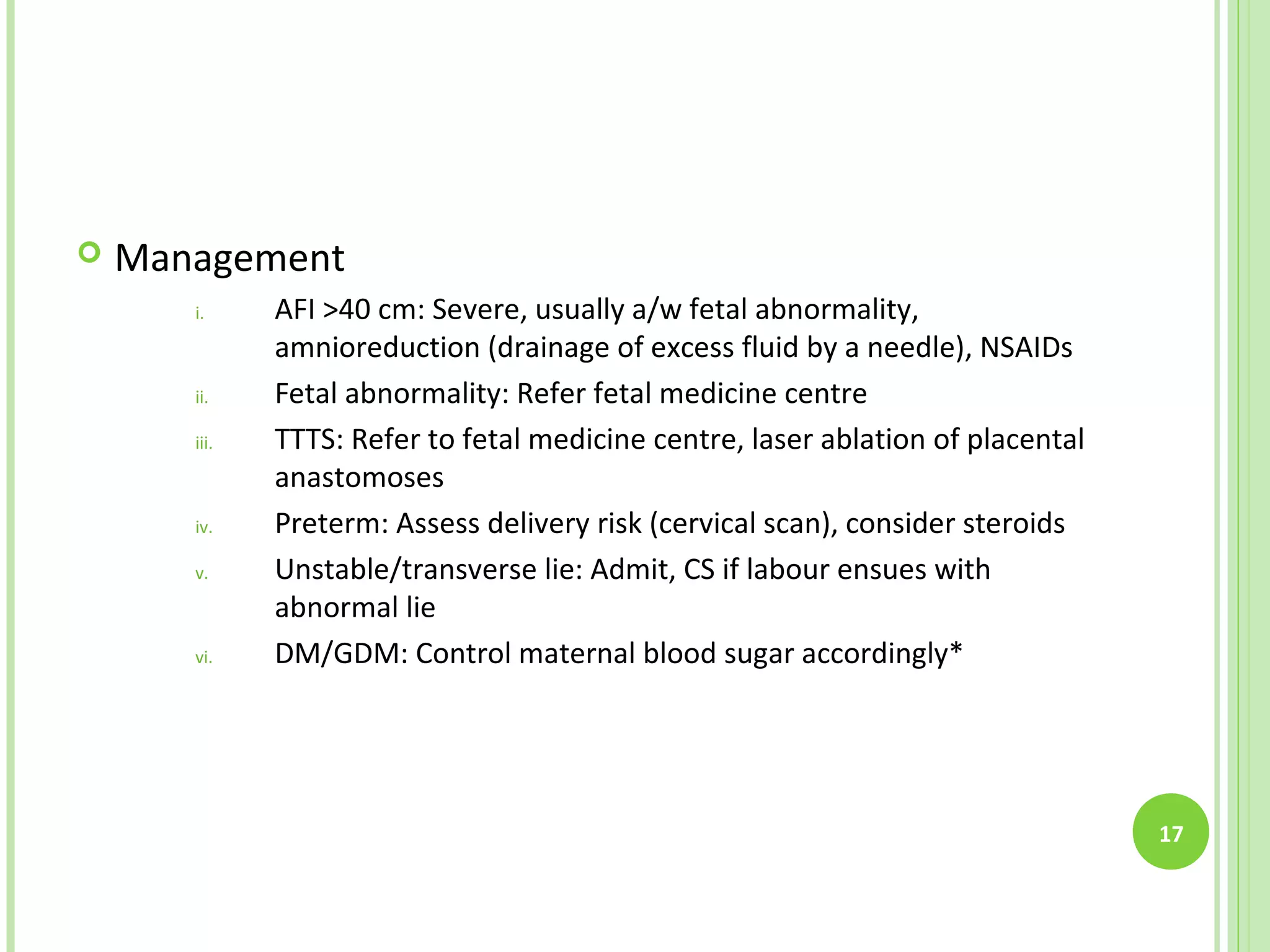
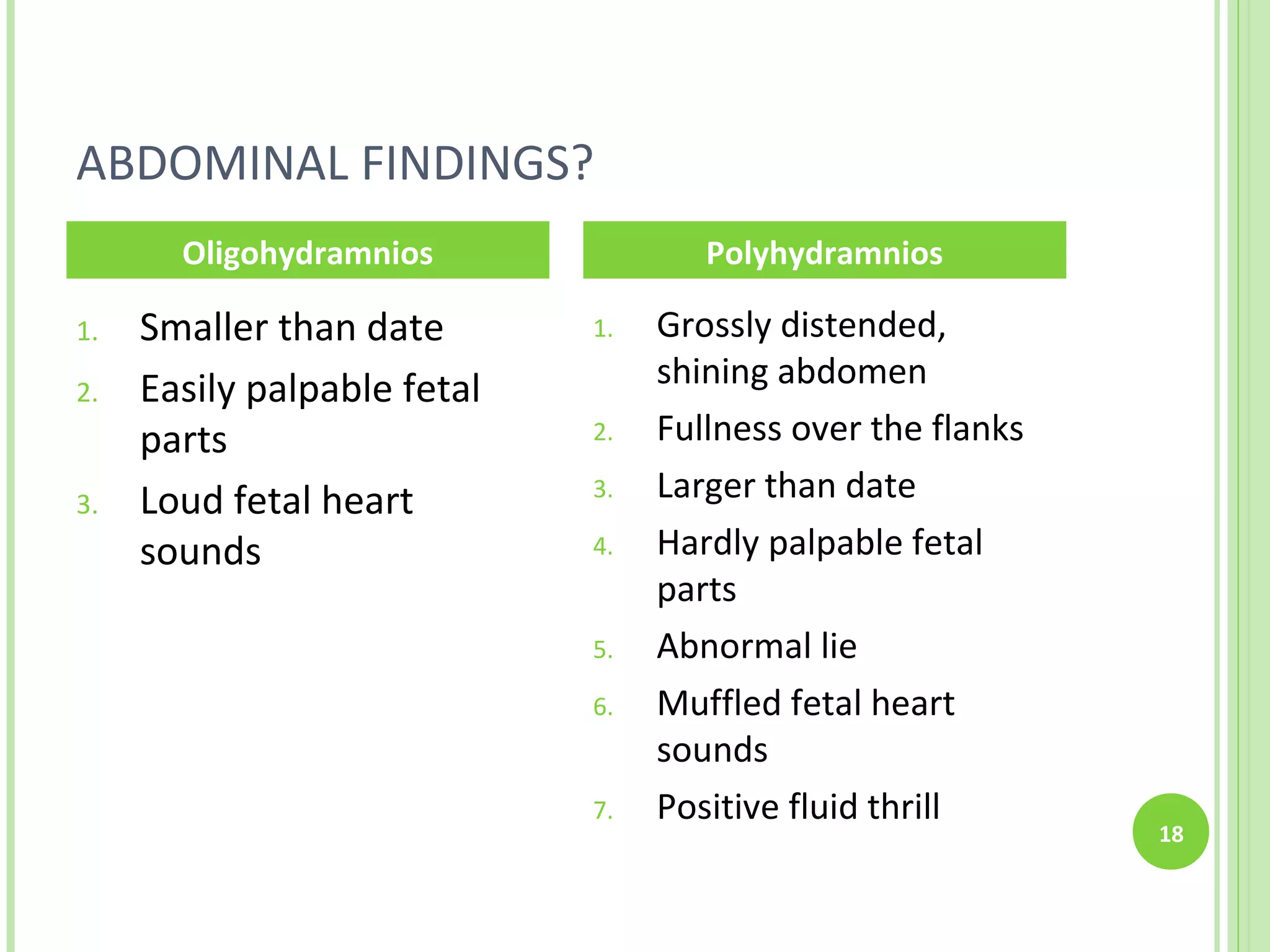
This document discusses fundal size discrepancies including being smaller or larger than dates. Being smaller than dates can be due to fetal issues like growth restriction or demise, or maternal issues like a wrong date. Differentials are investigated by ultrasound. Being larger than dates can be due to multiple pregnancies, macrosomia, or a wrong date. Oligohydramnios and polyhydramnios are also discussed, including their definitions, causes, investigations, complications and management. Intrauterine growth restriction is explained in detail with causes, investigations and complications.