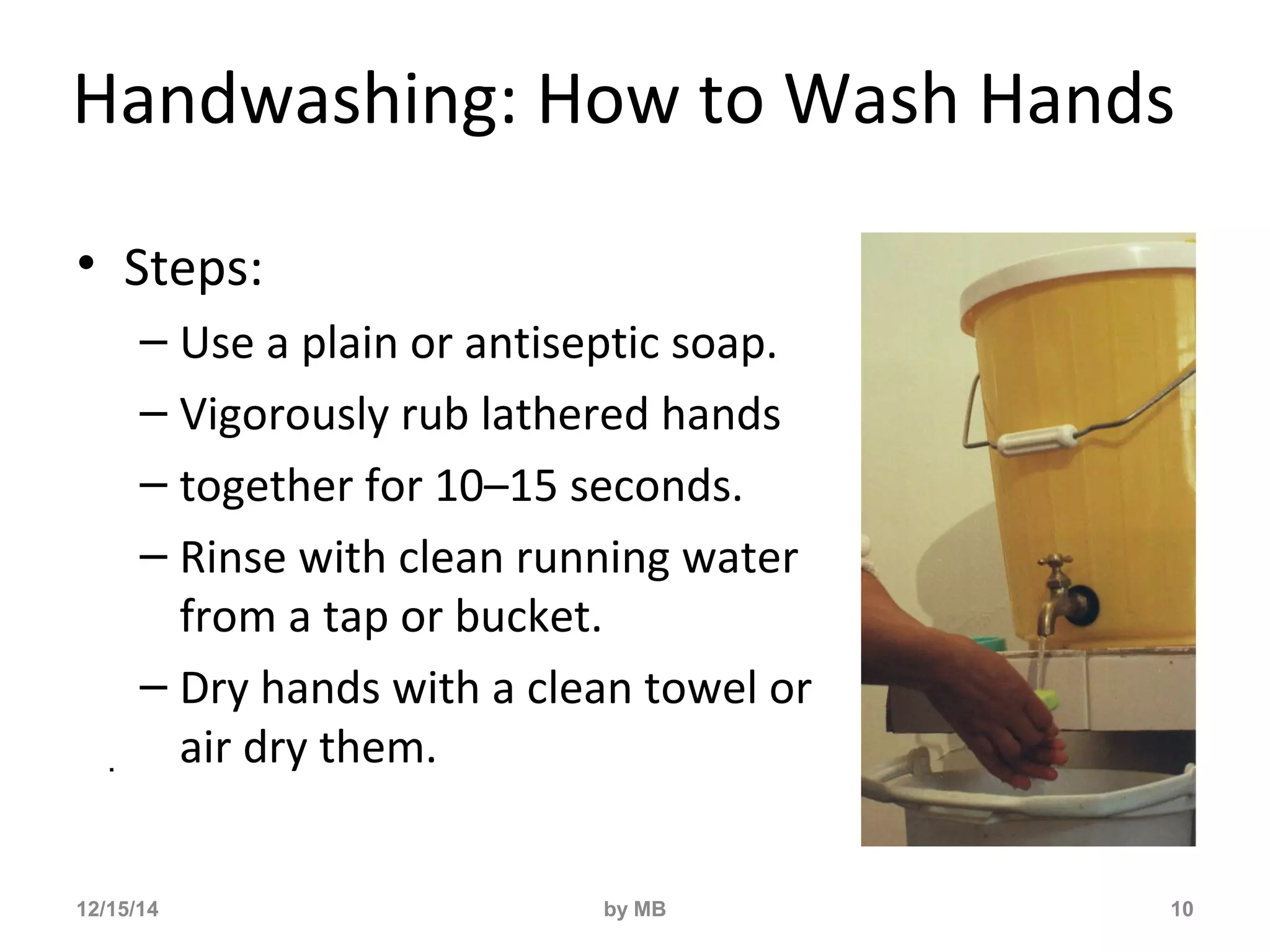
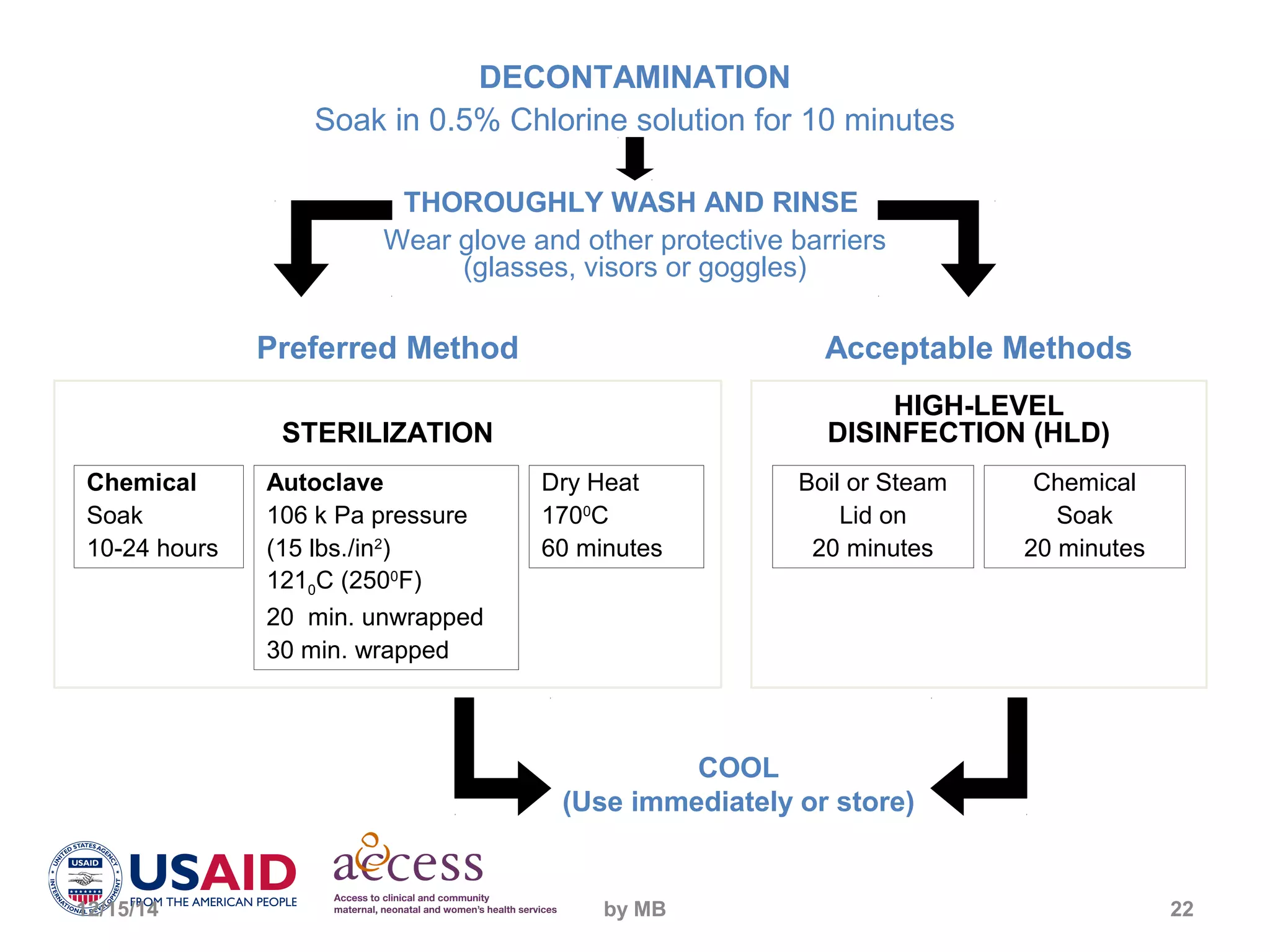
This document outlines best practices for infection prevention including describing the disease transmission cycle, key principles of infection prevention, and proper handwashing, antisepsis, use of personal protective equipment, safe handling of sharps, instrument processing, and waste disposal. It emphasizes that rigorous adherence to infection prevention practices such as handwashing, use of antiseptics and protective equipment, and safe disposal of contaminated waste and needles can significantly reduce the risk of infection for both healthcare staff and patients.