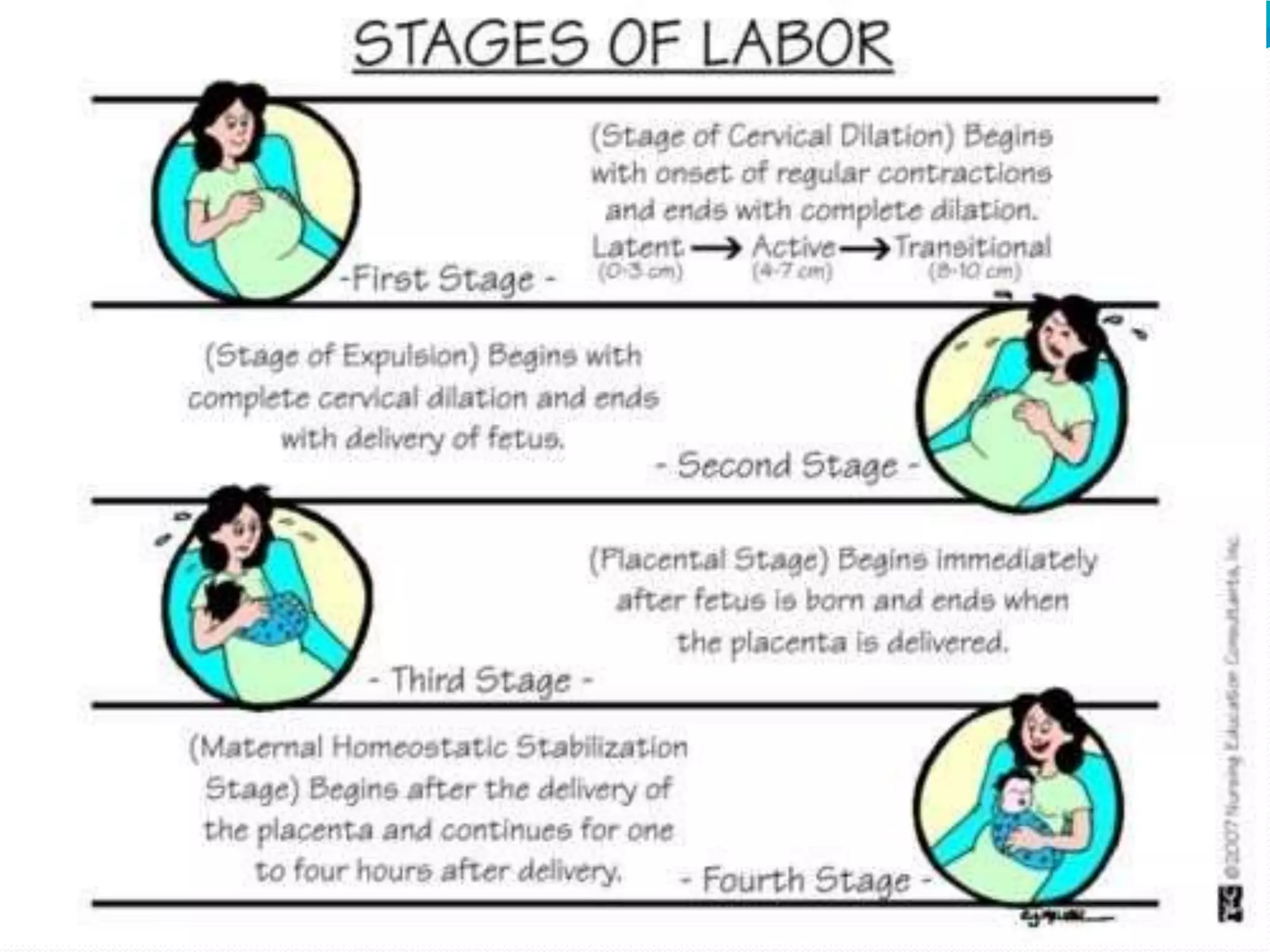
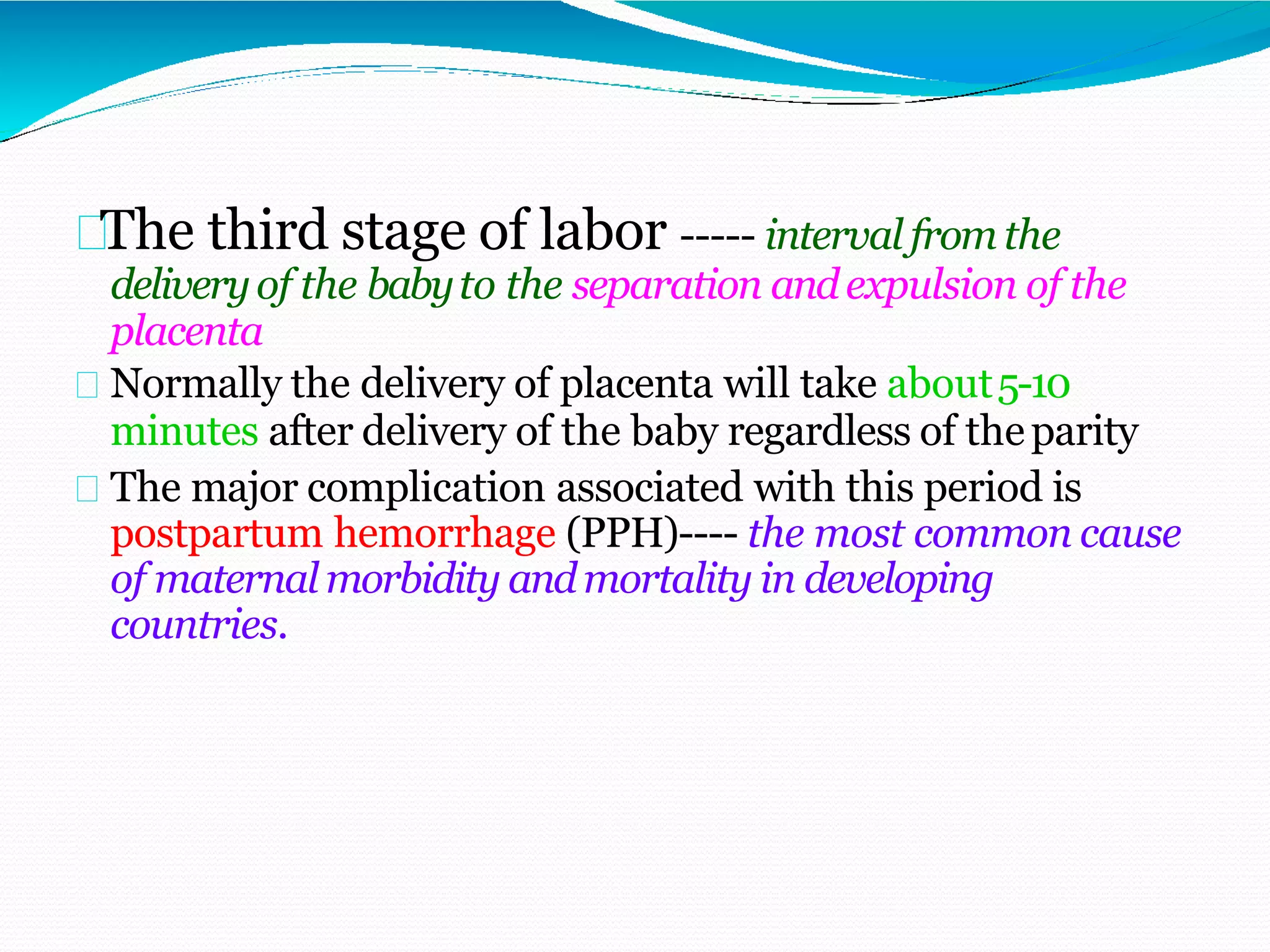
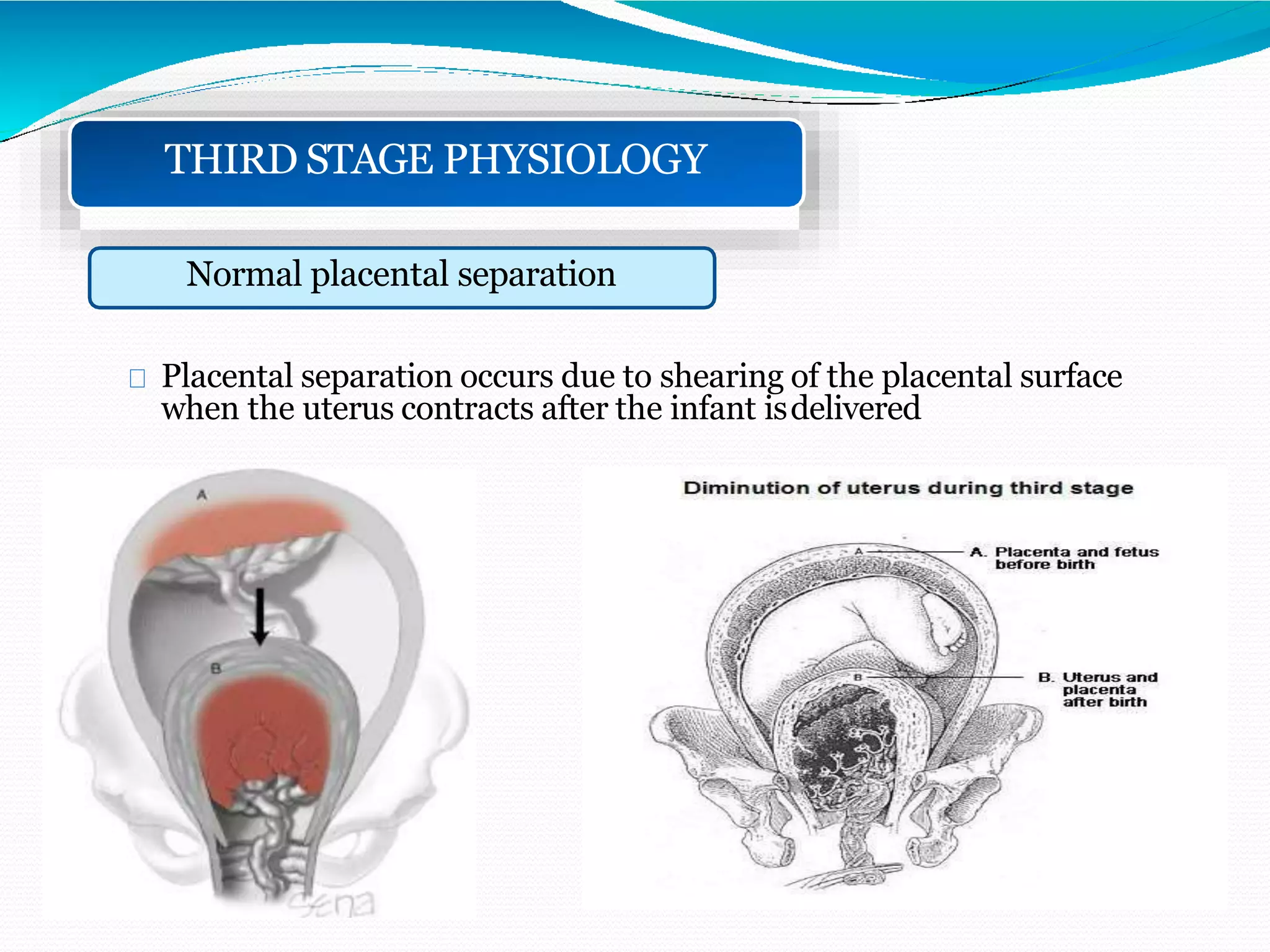
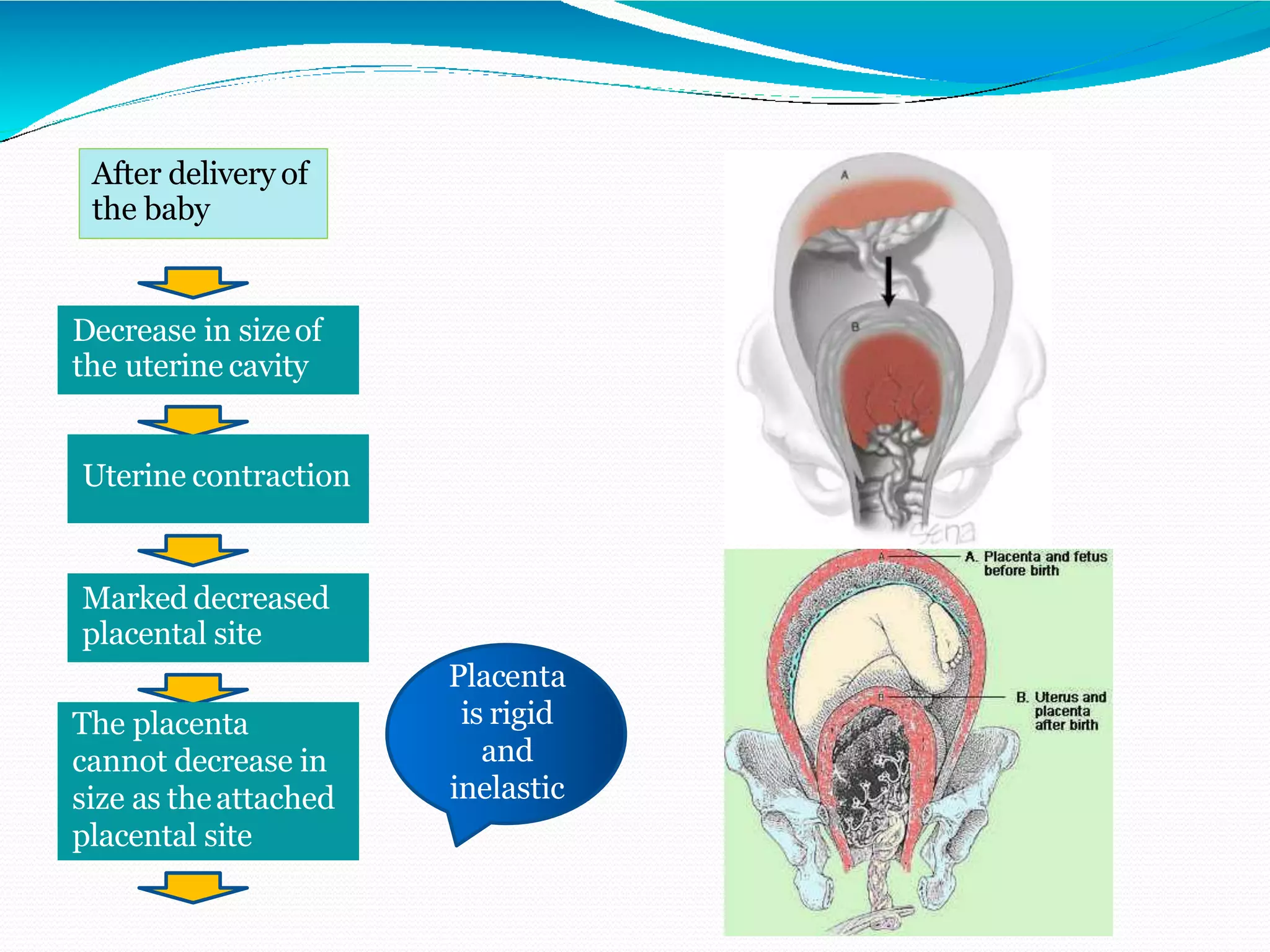
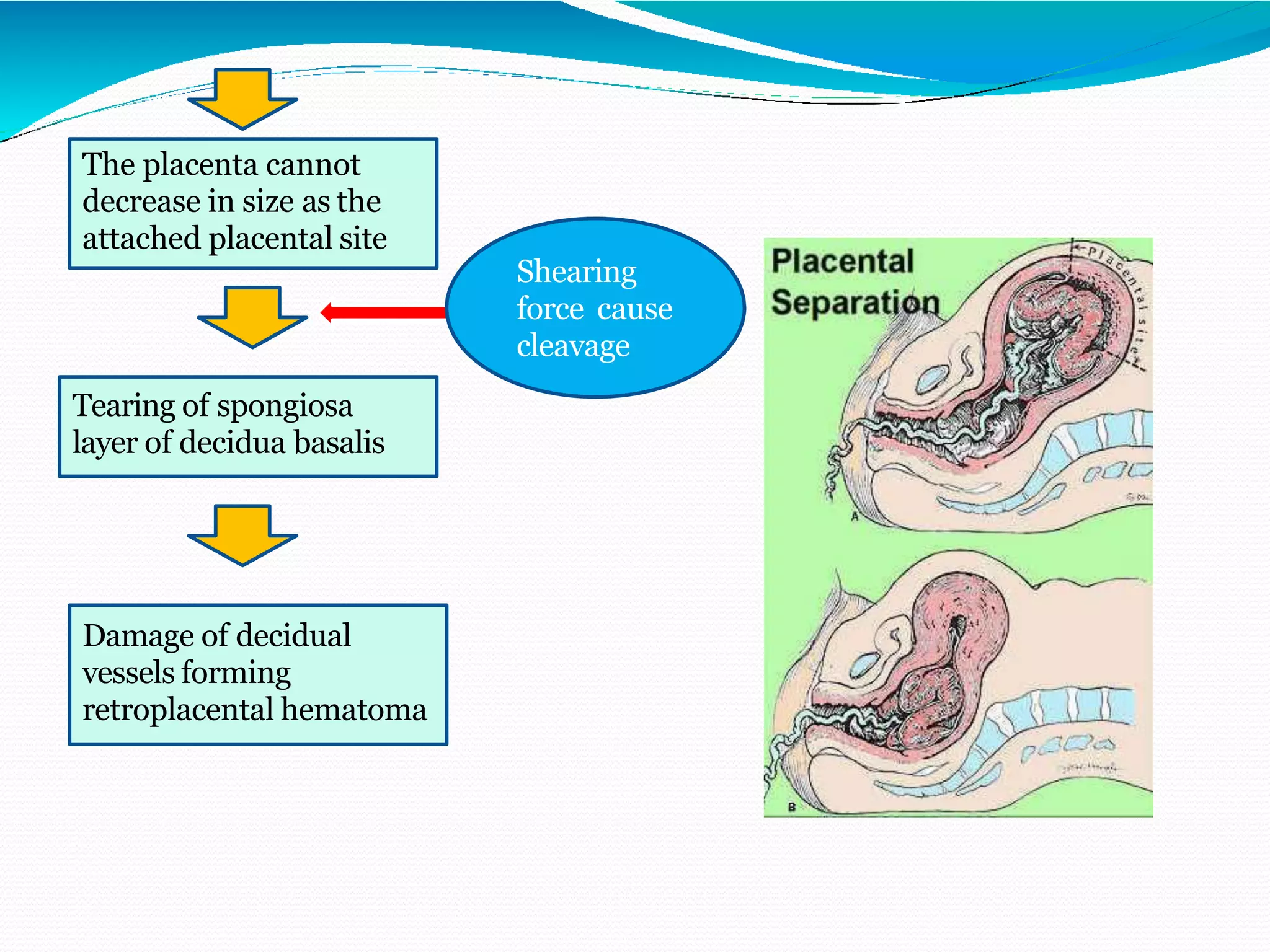
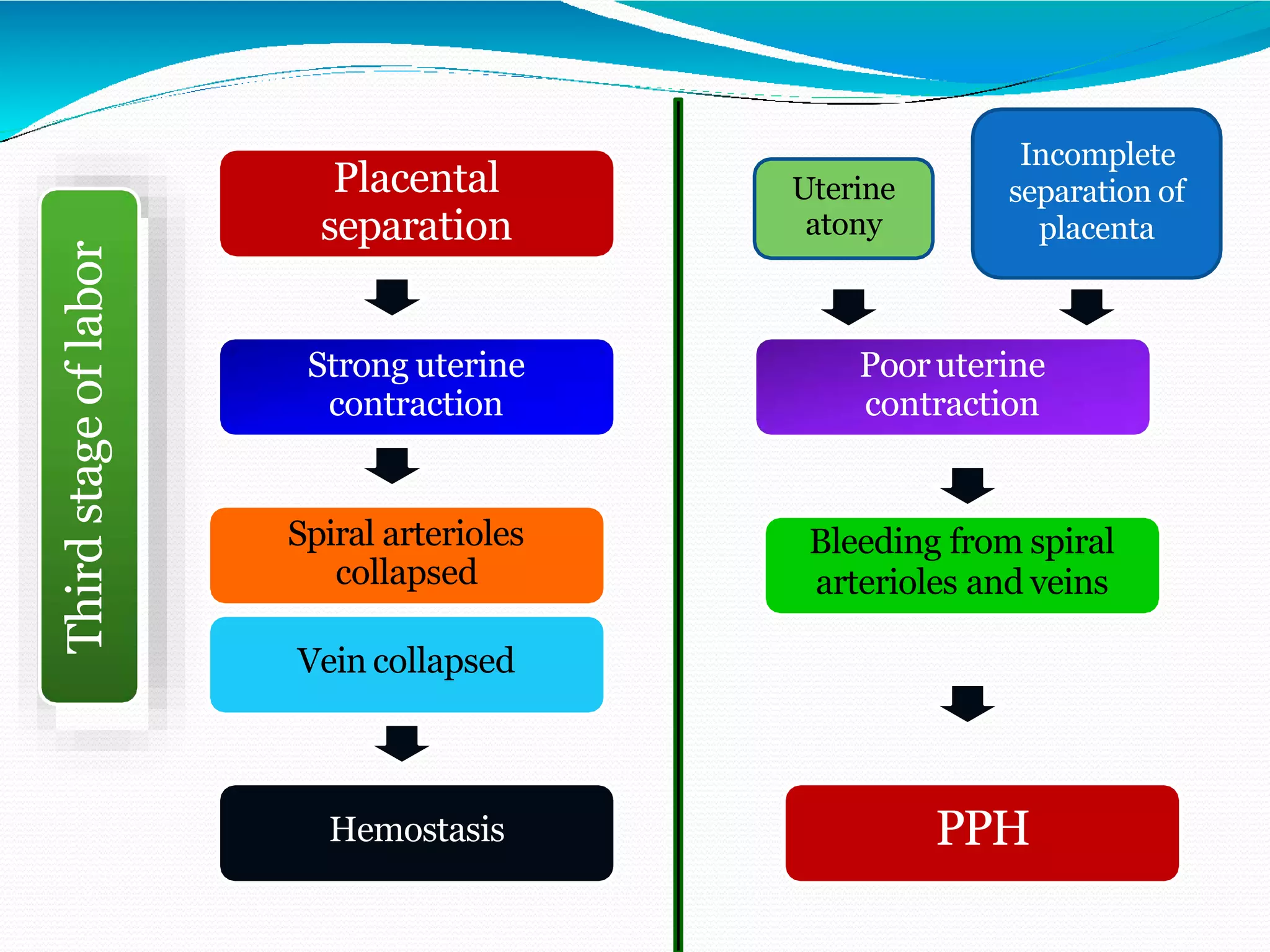
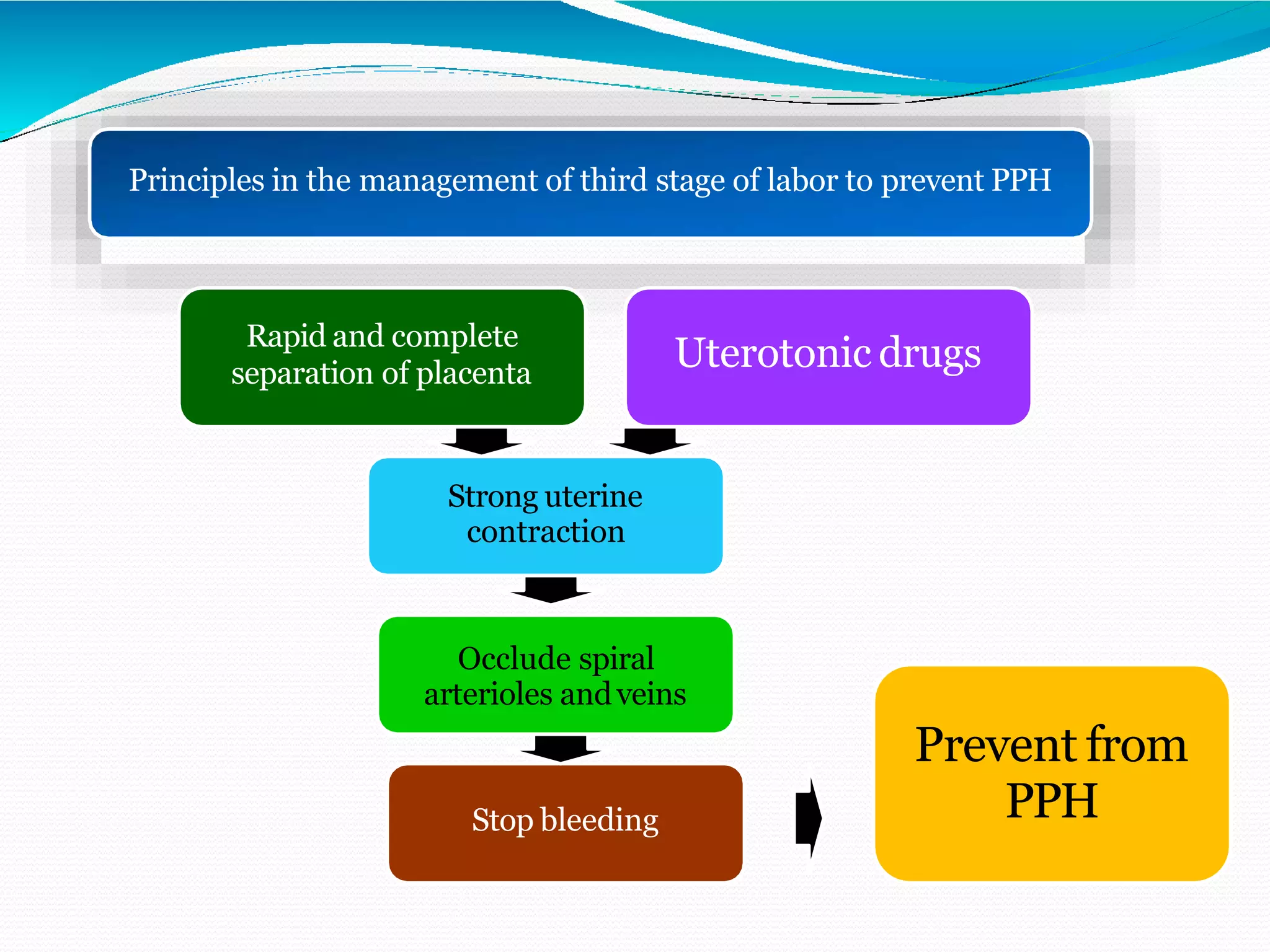
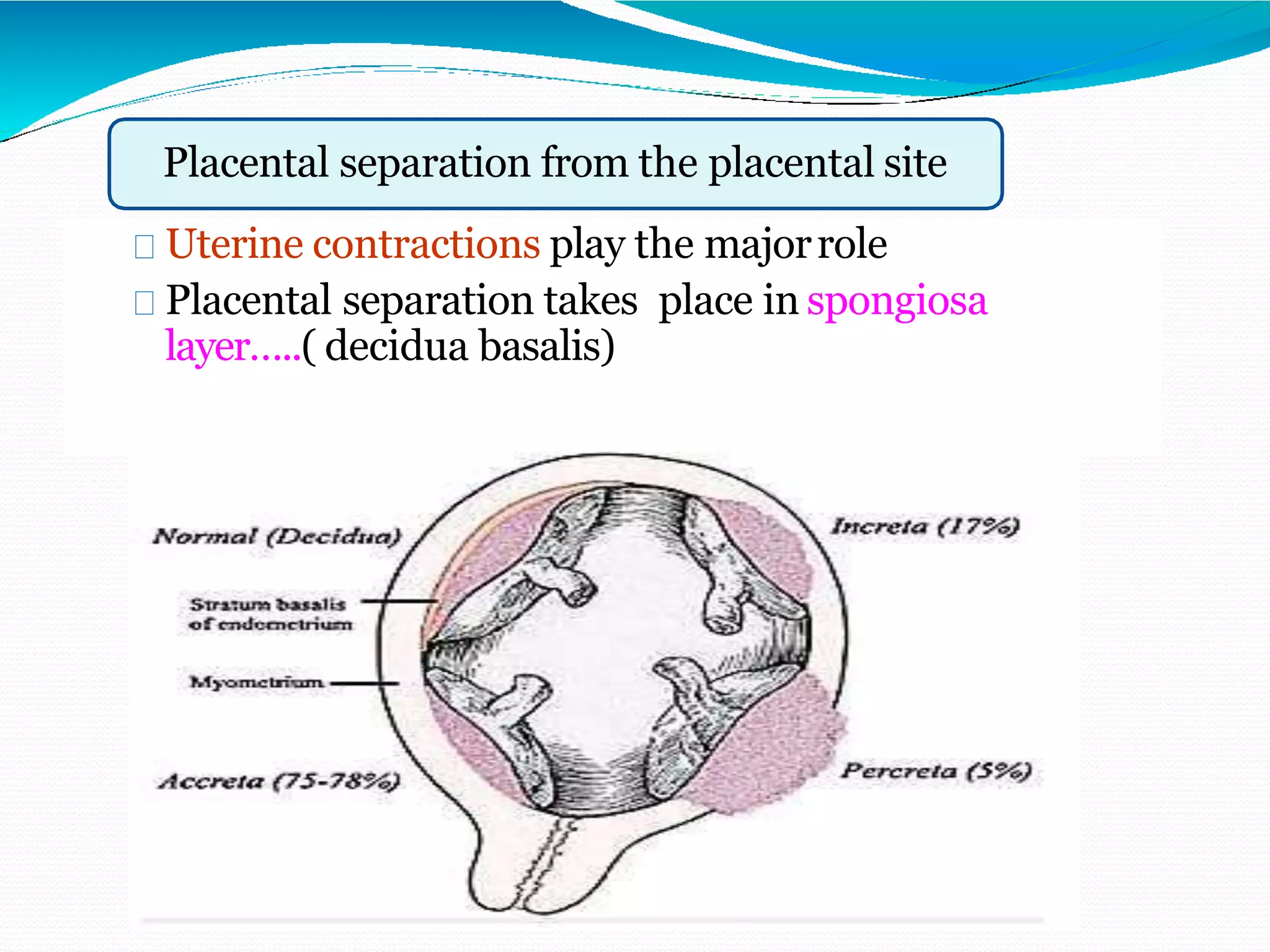
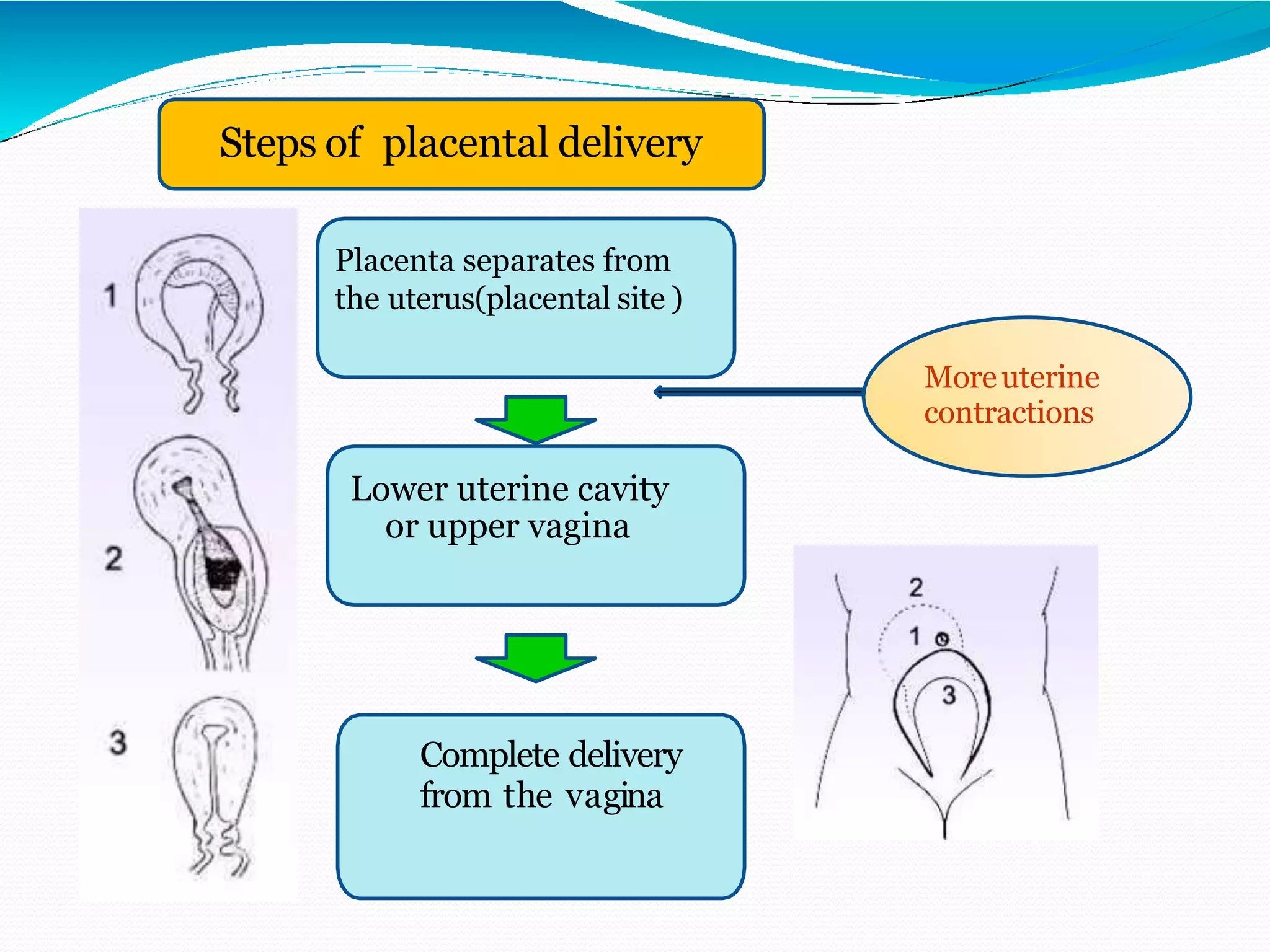
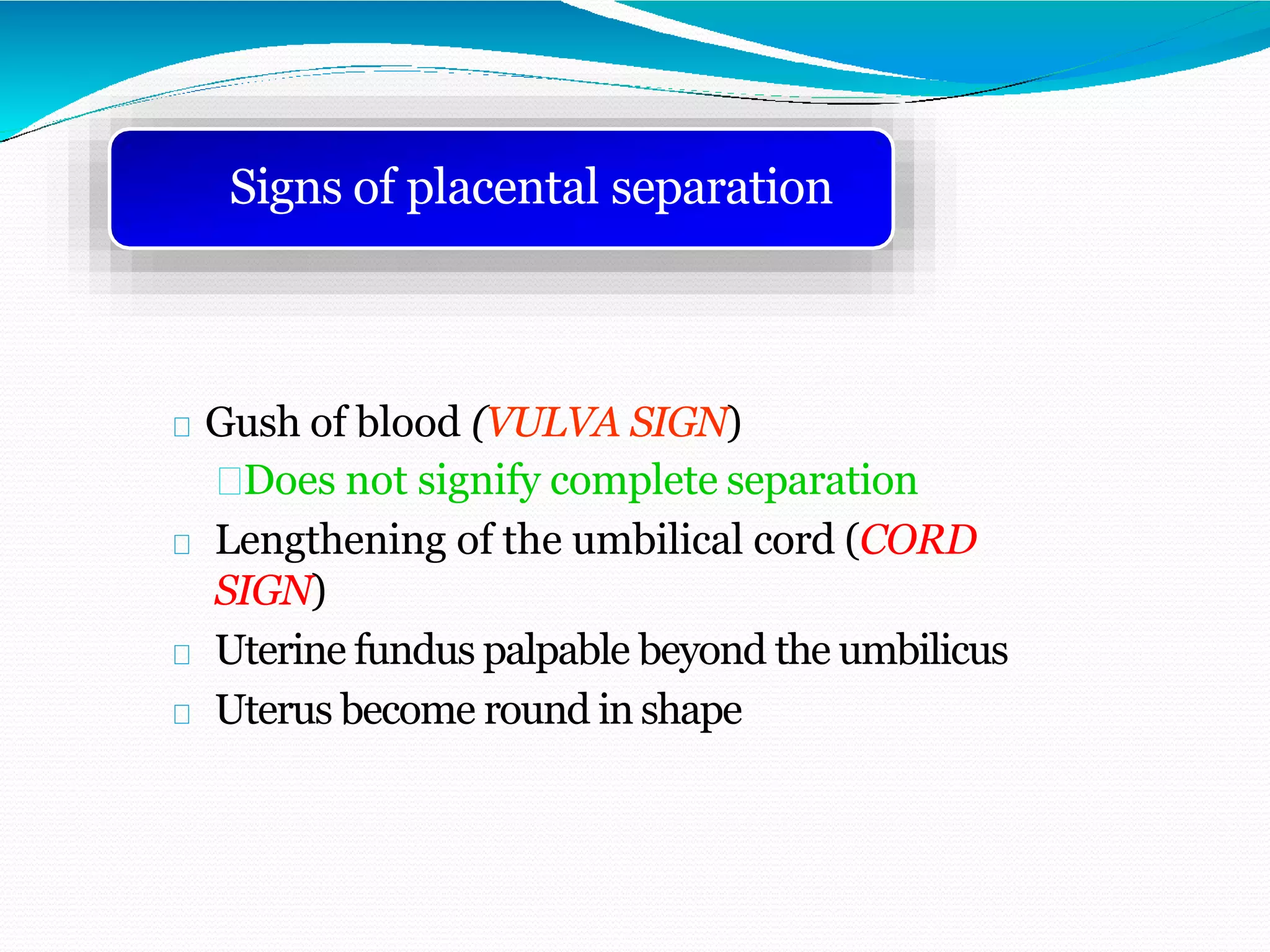
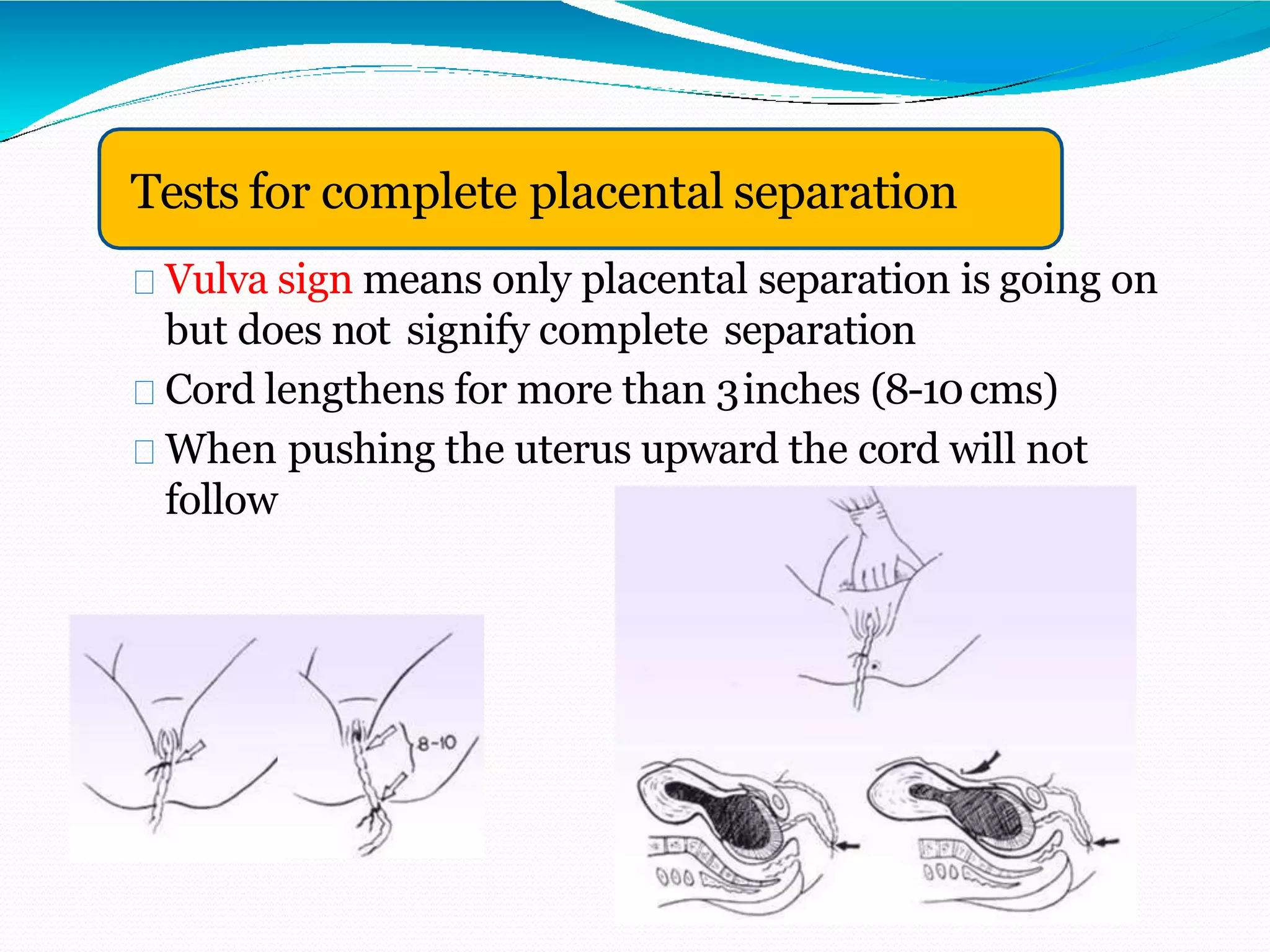
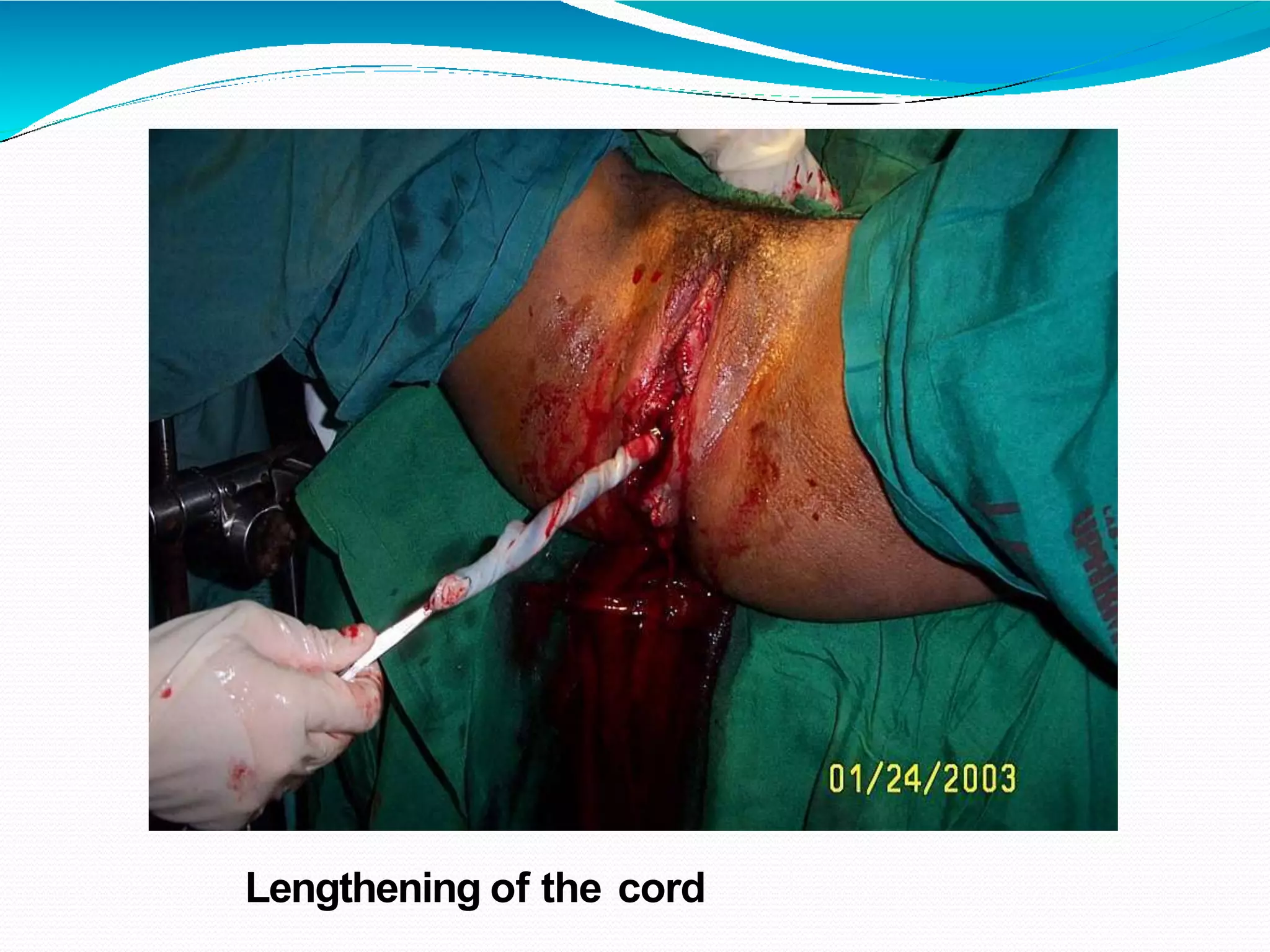
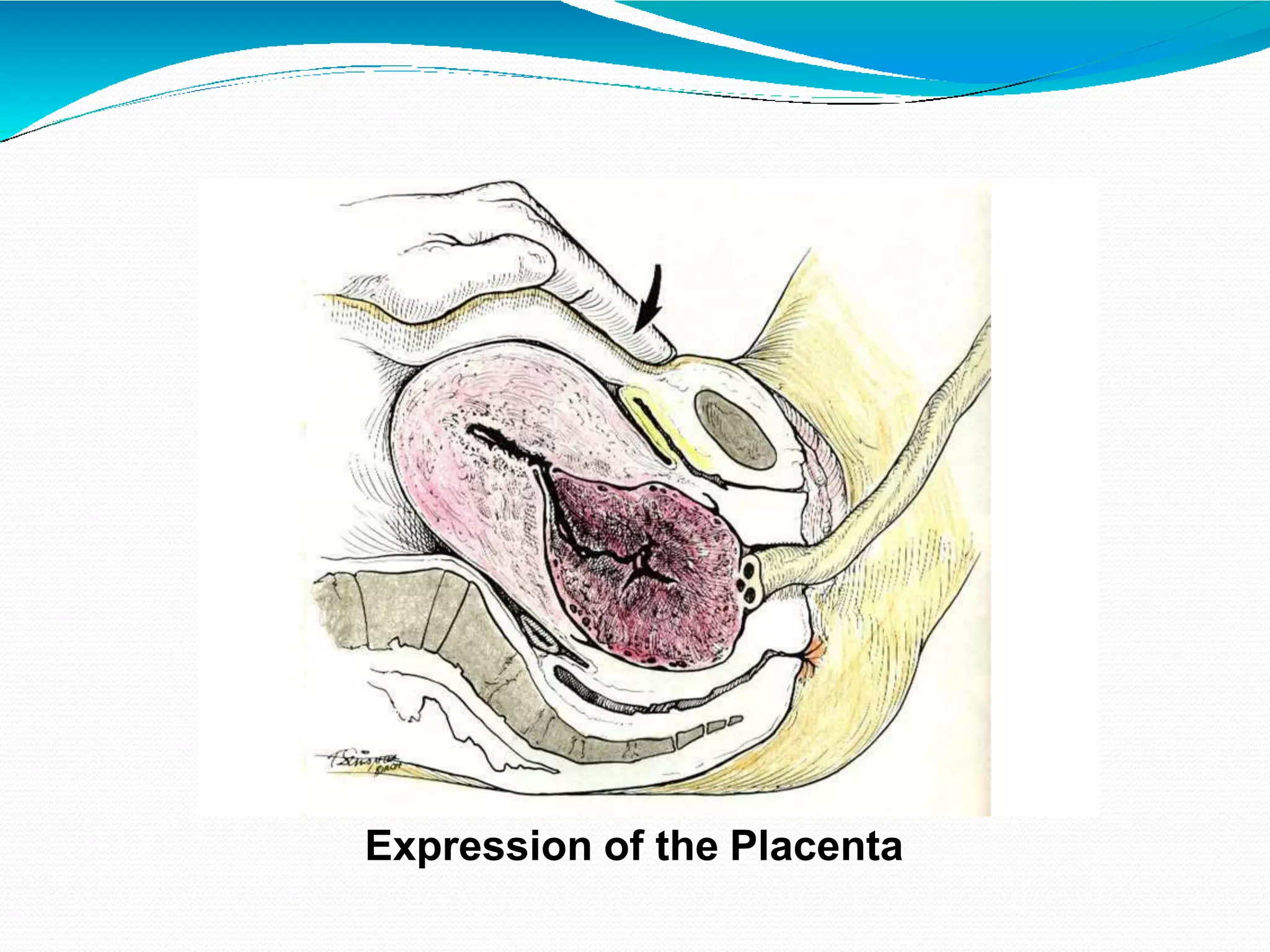
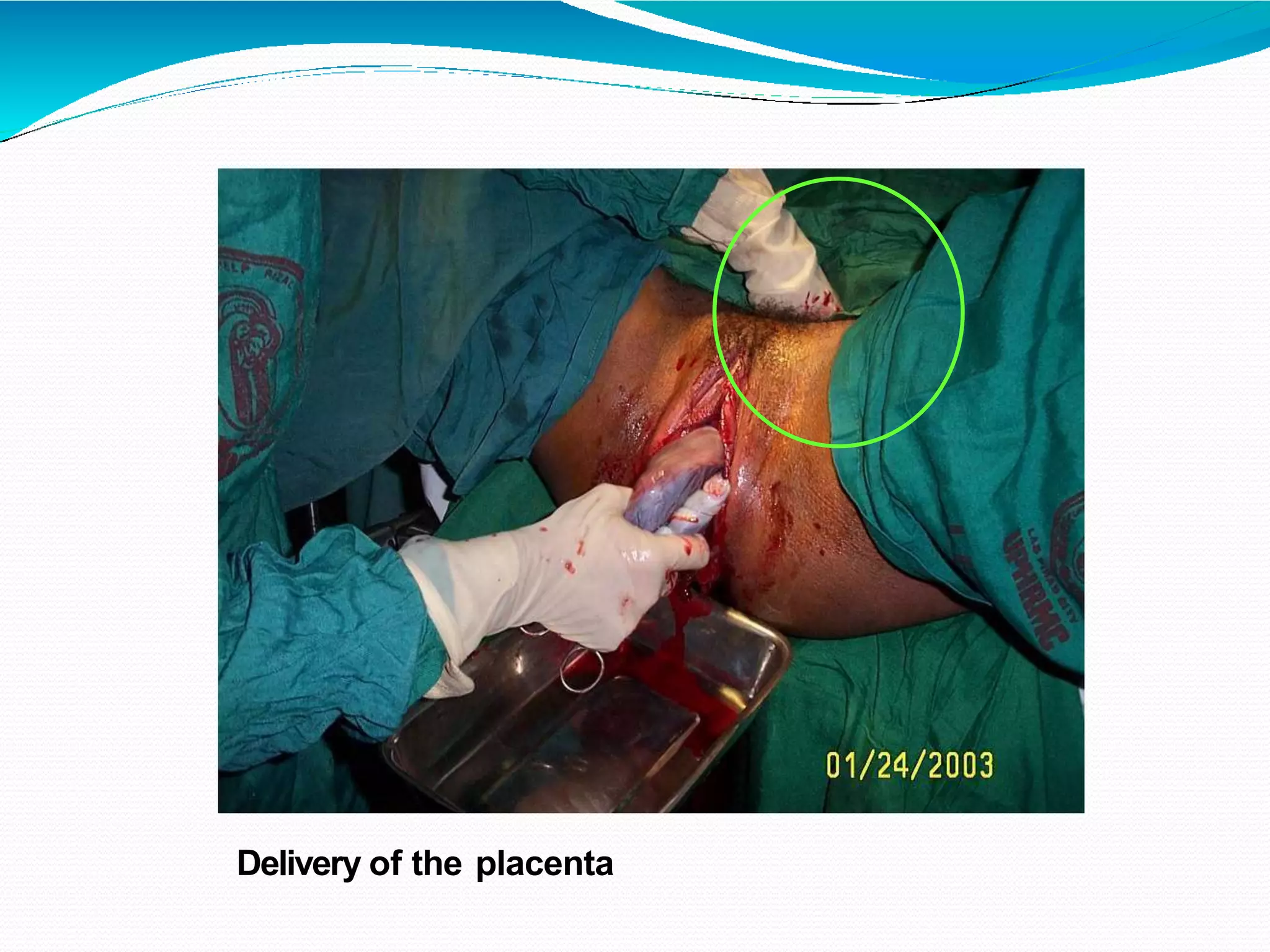
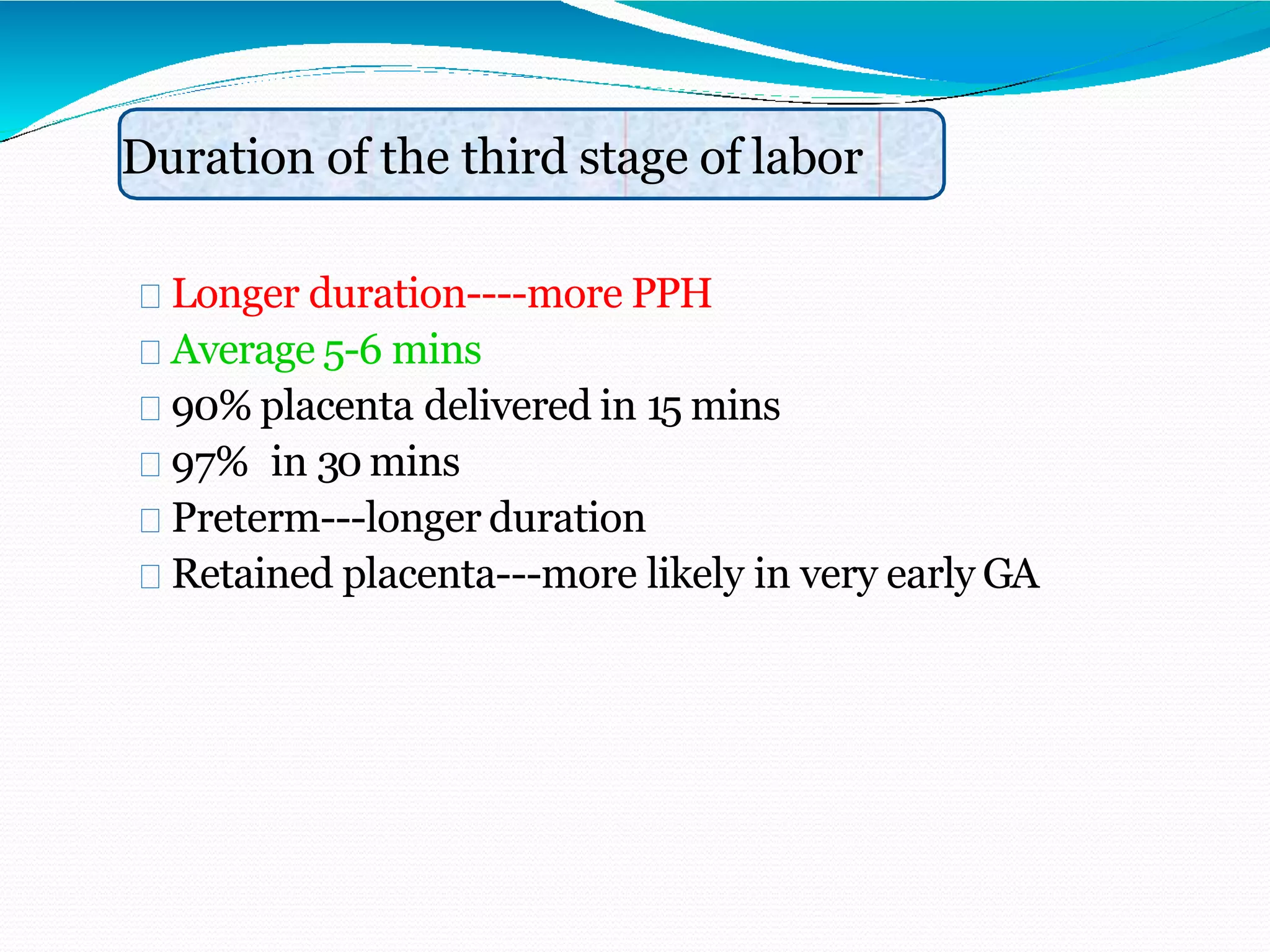
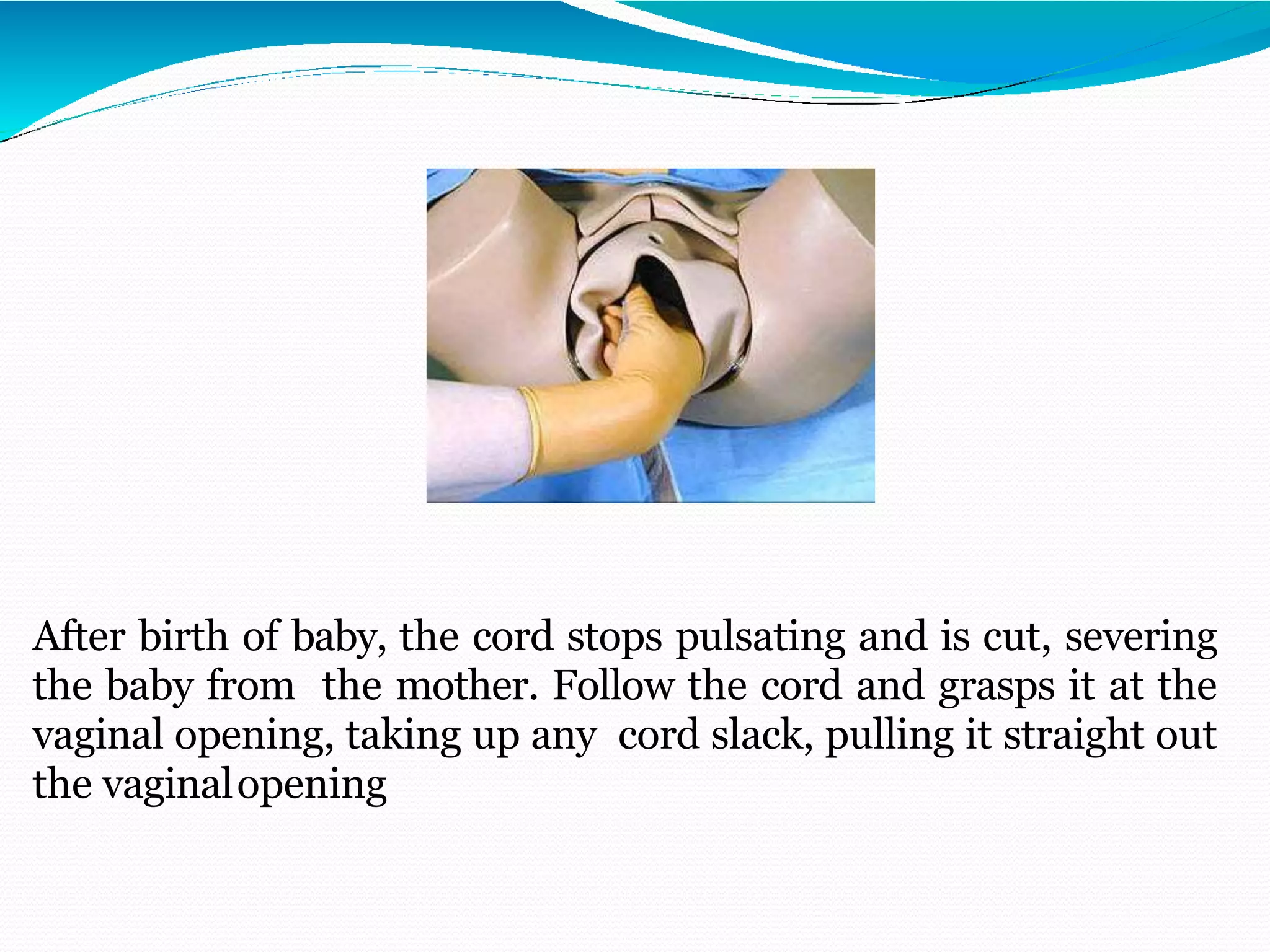
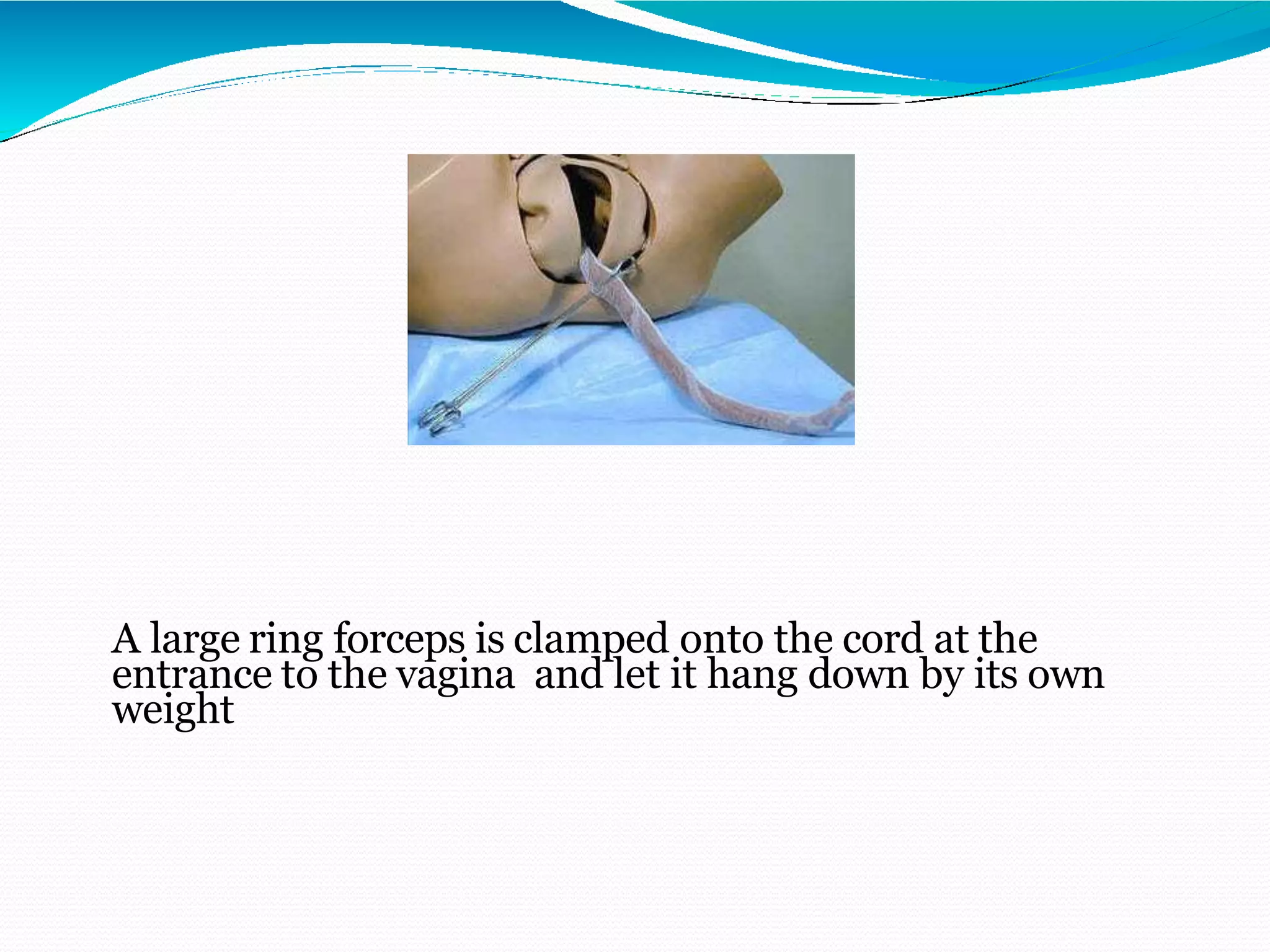
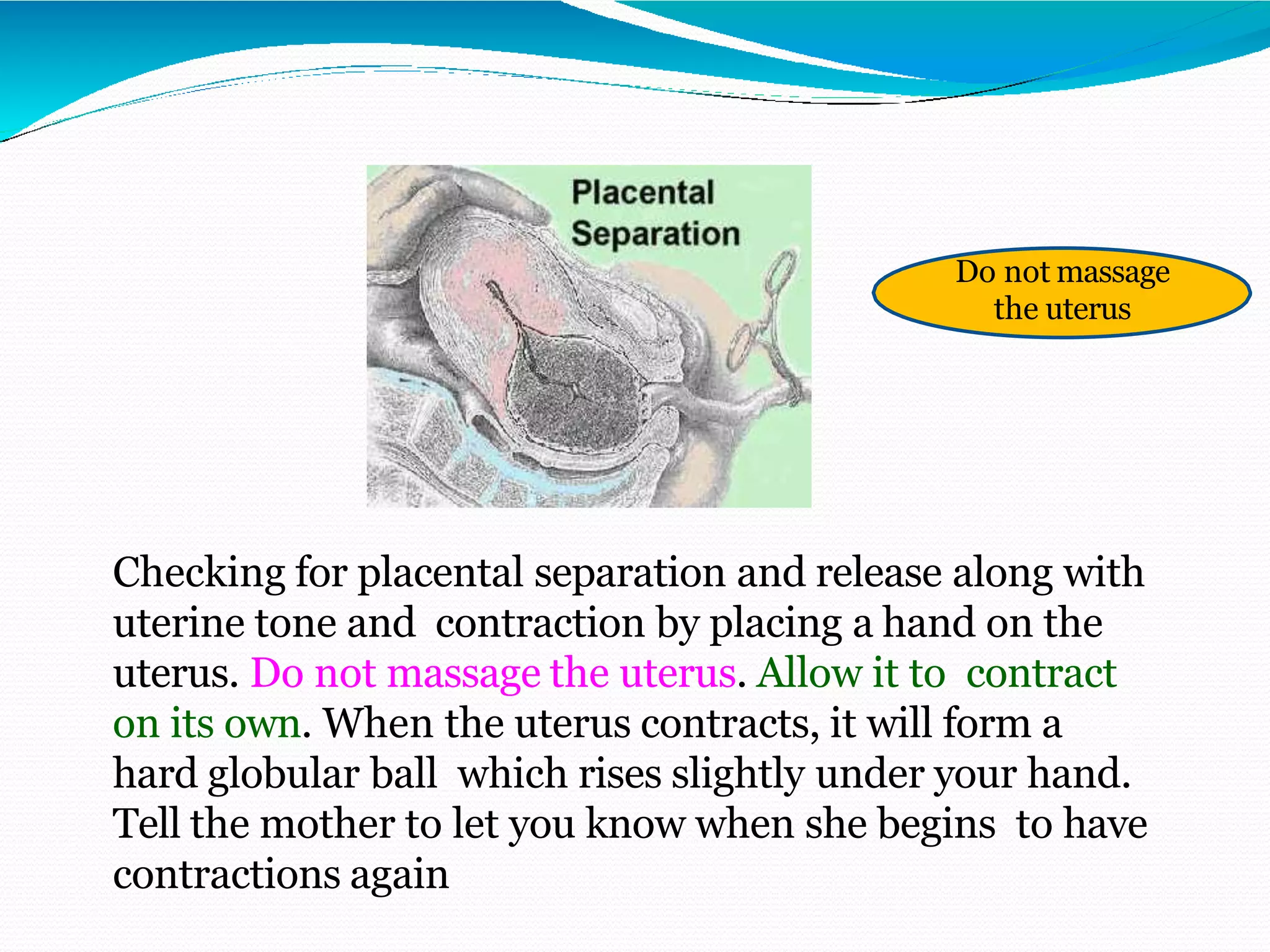
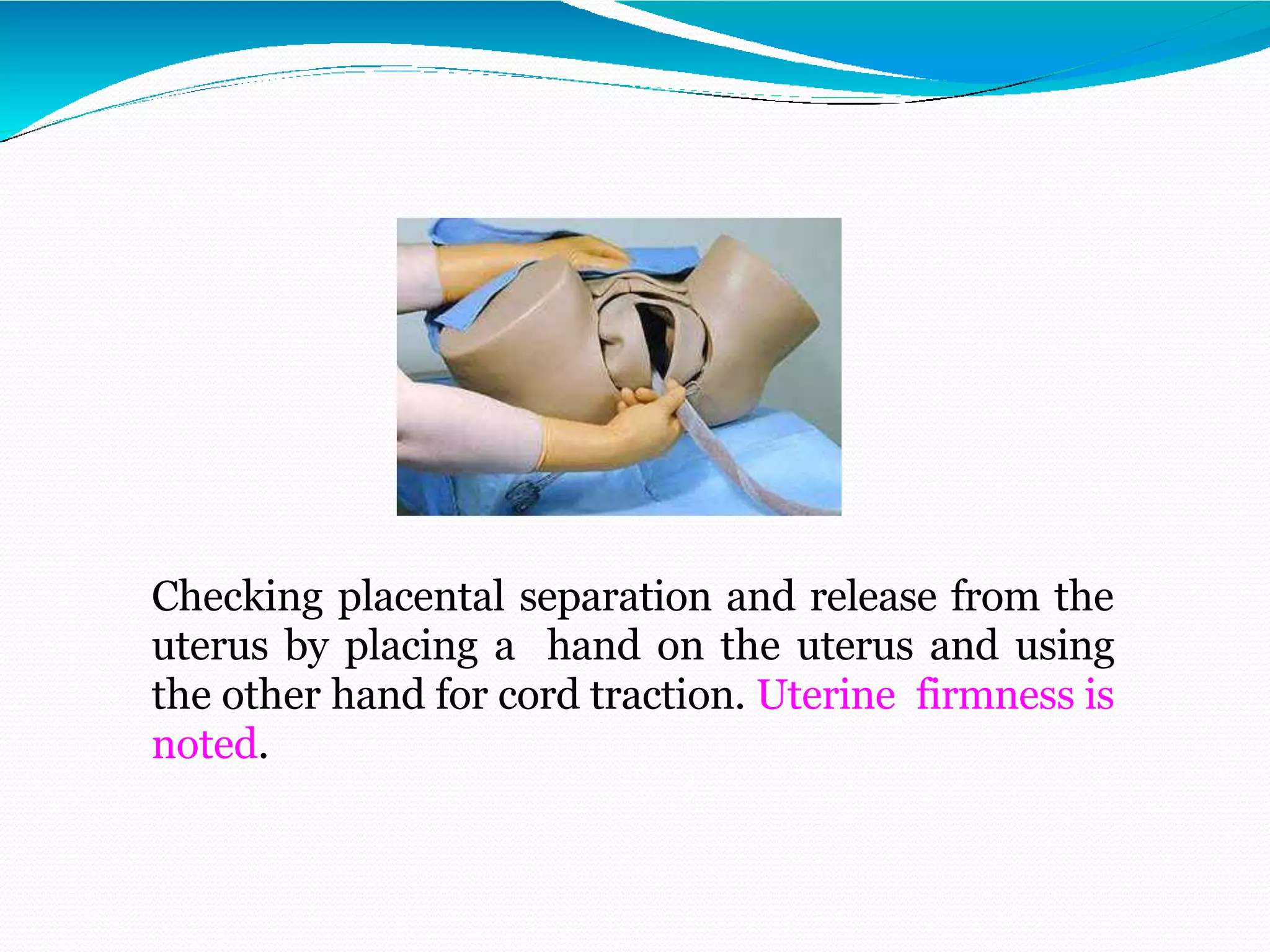
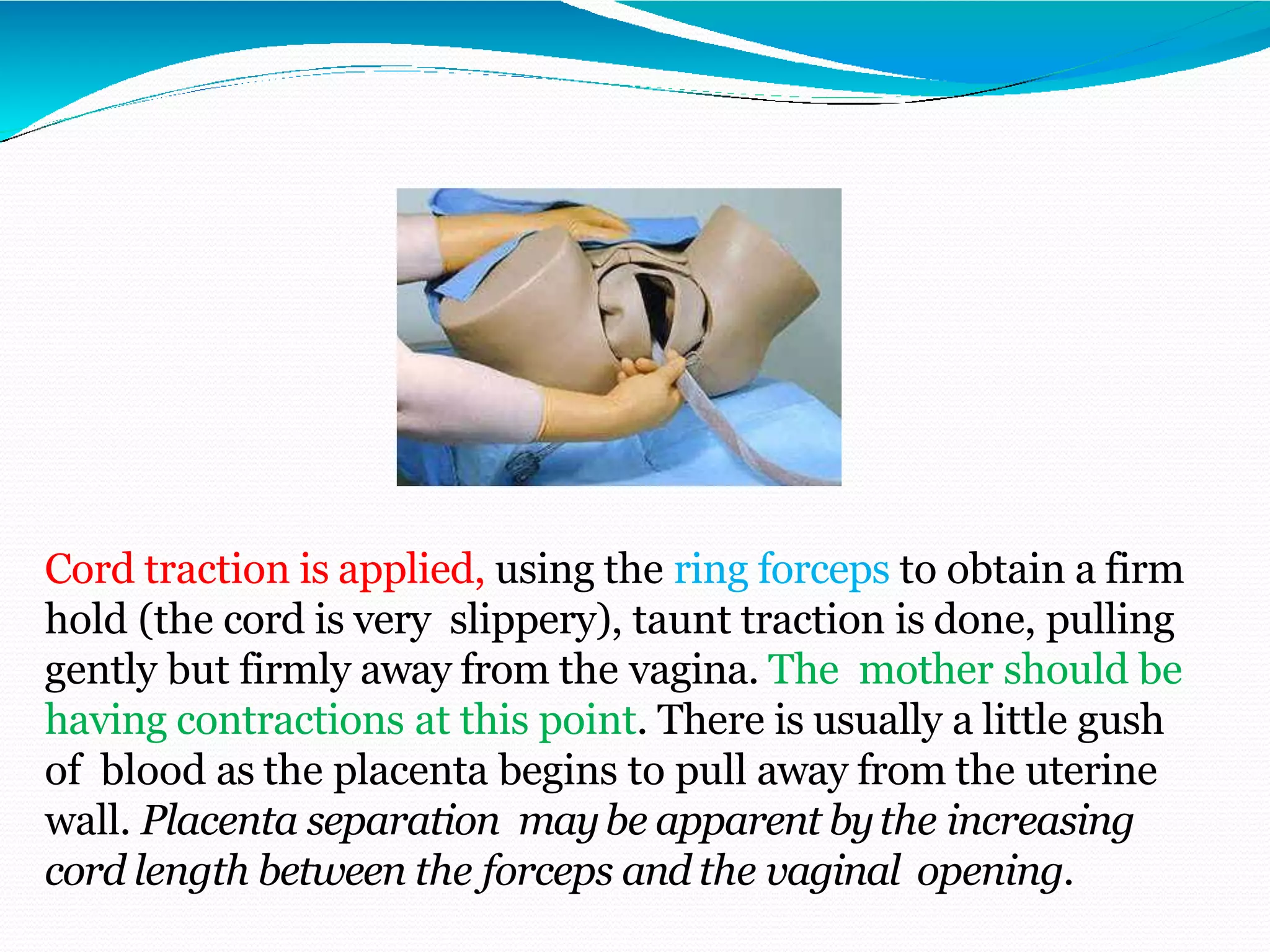
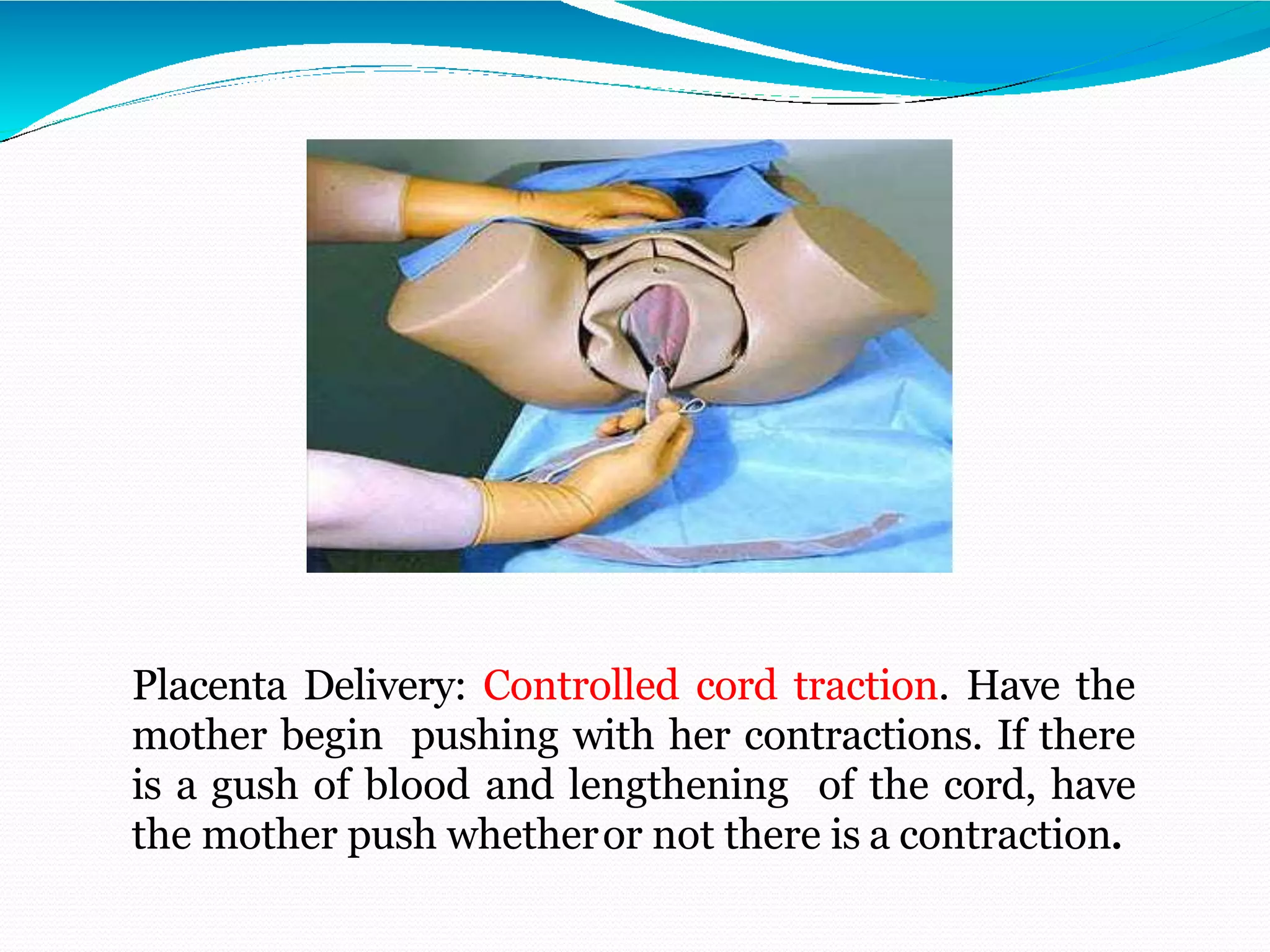
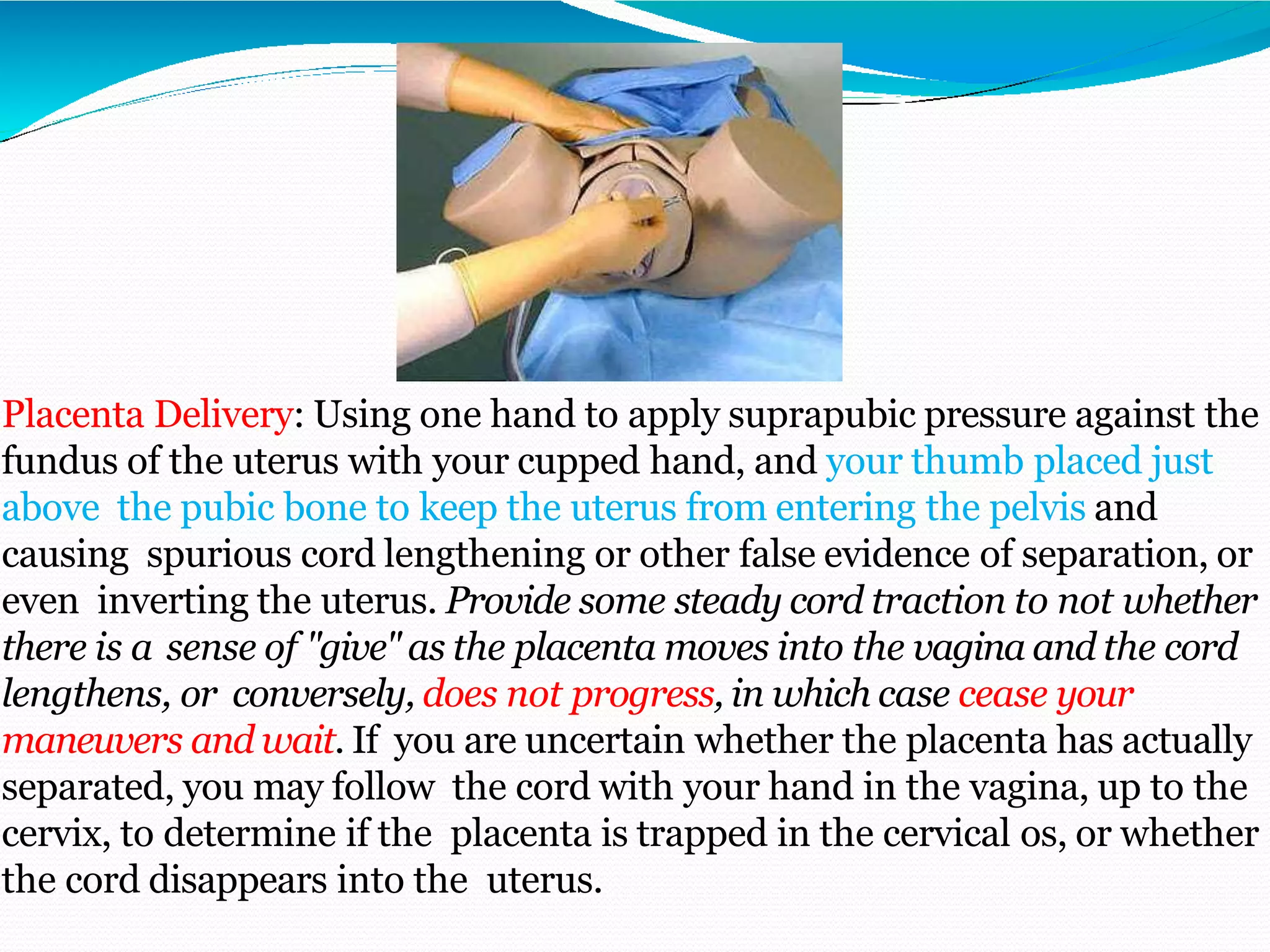
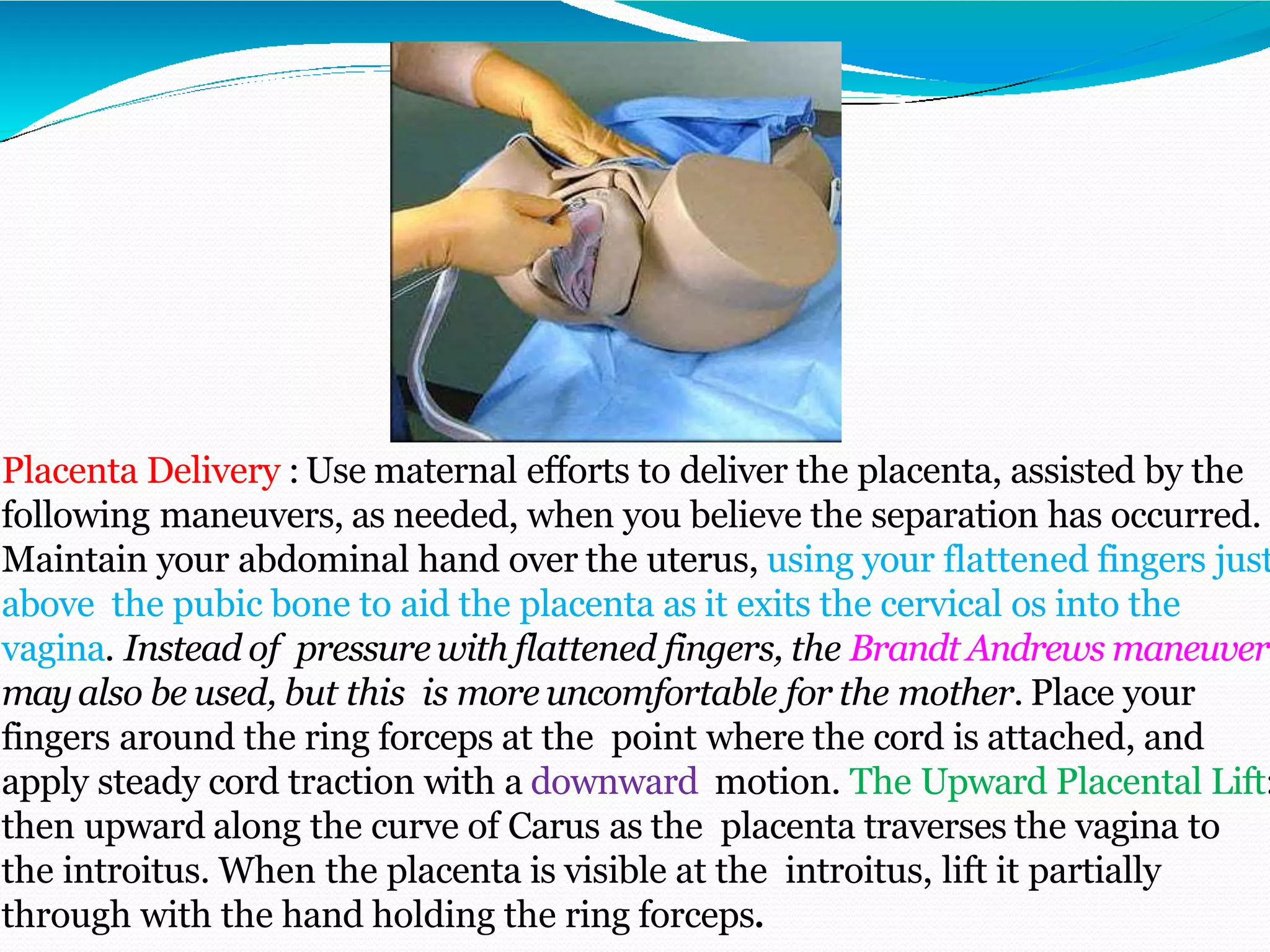
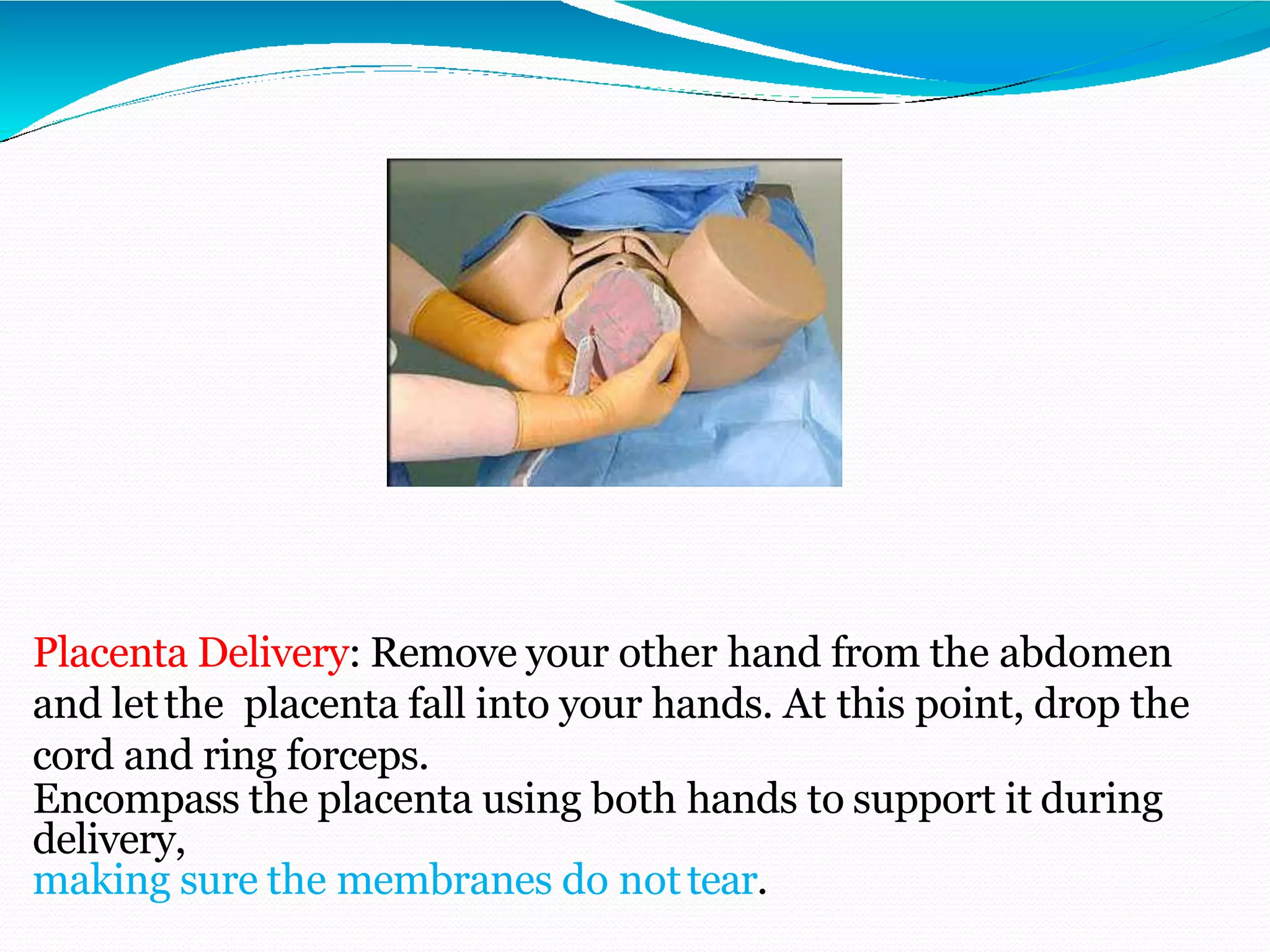
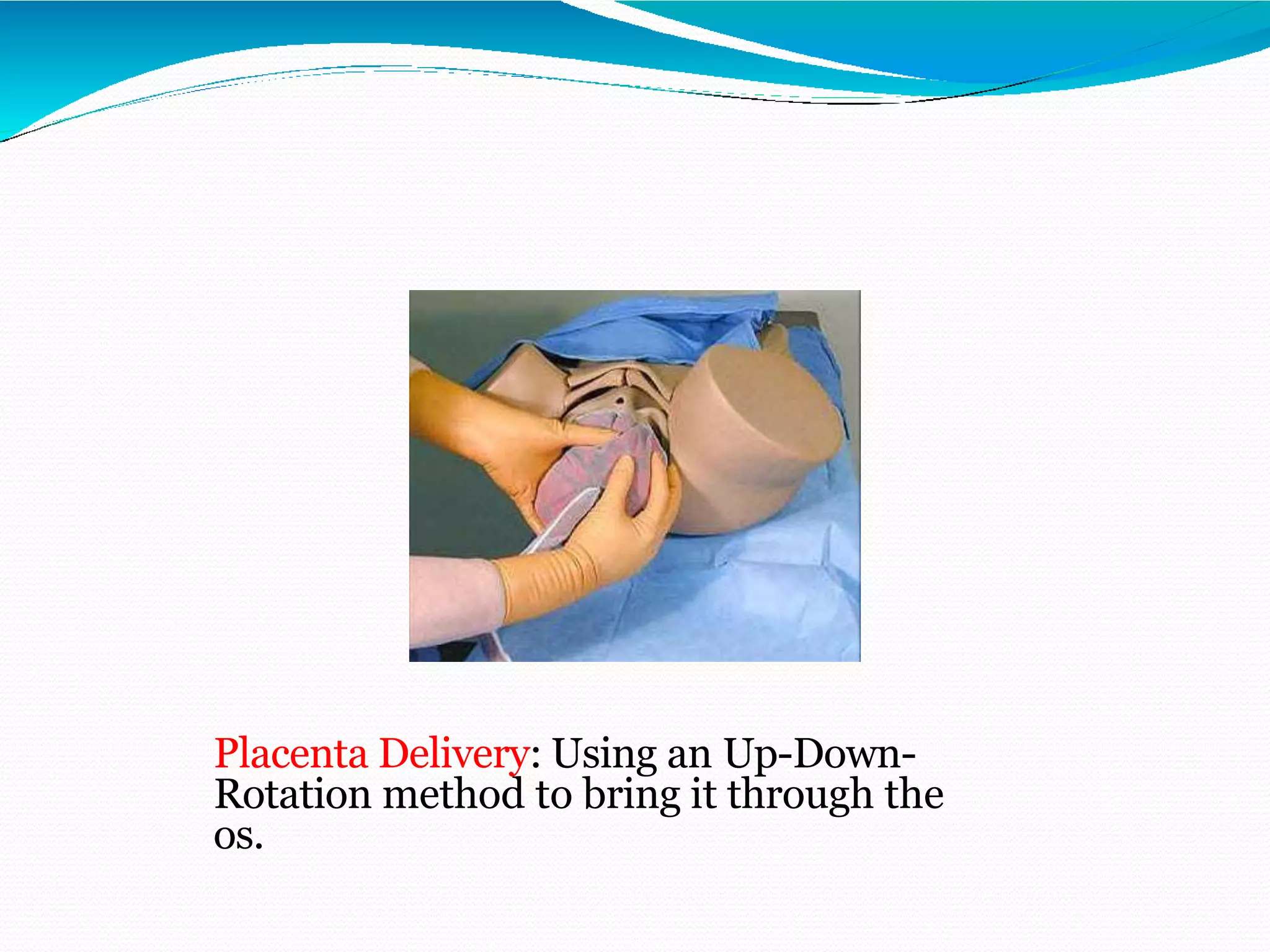
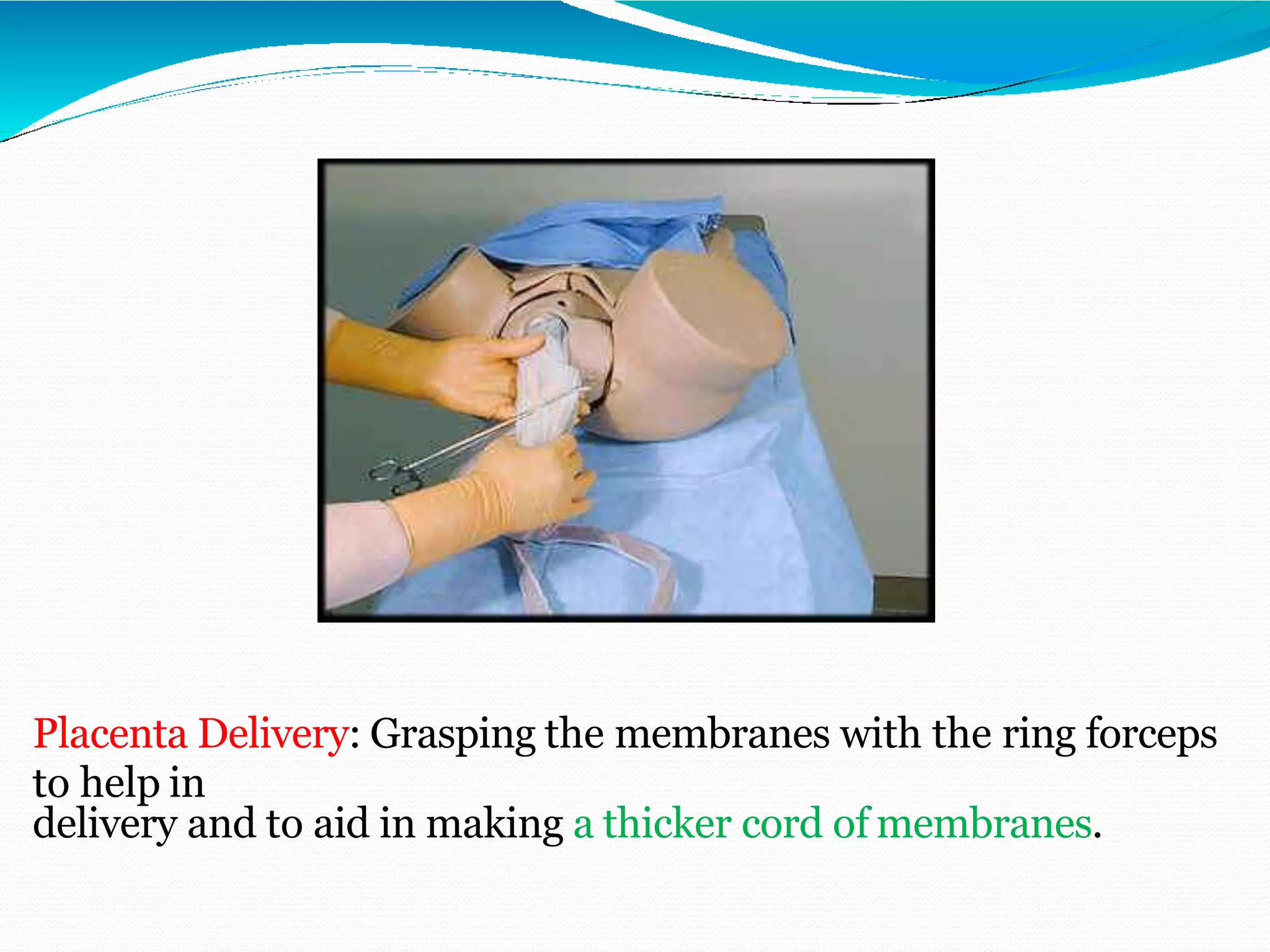
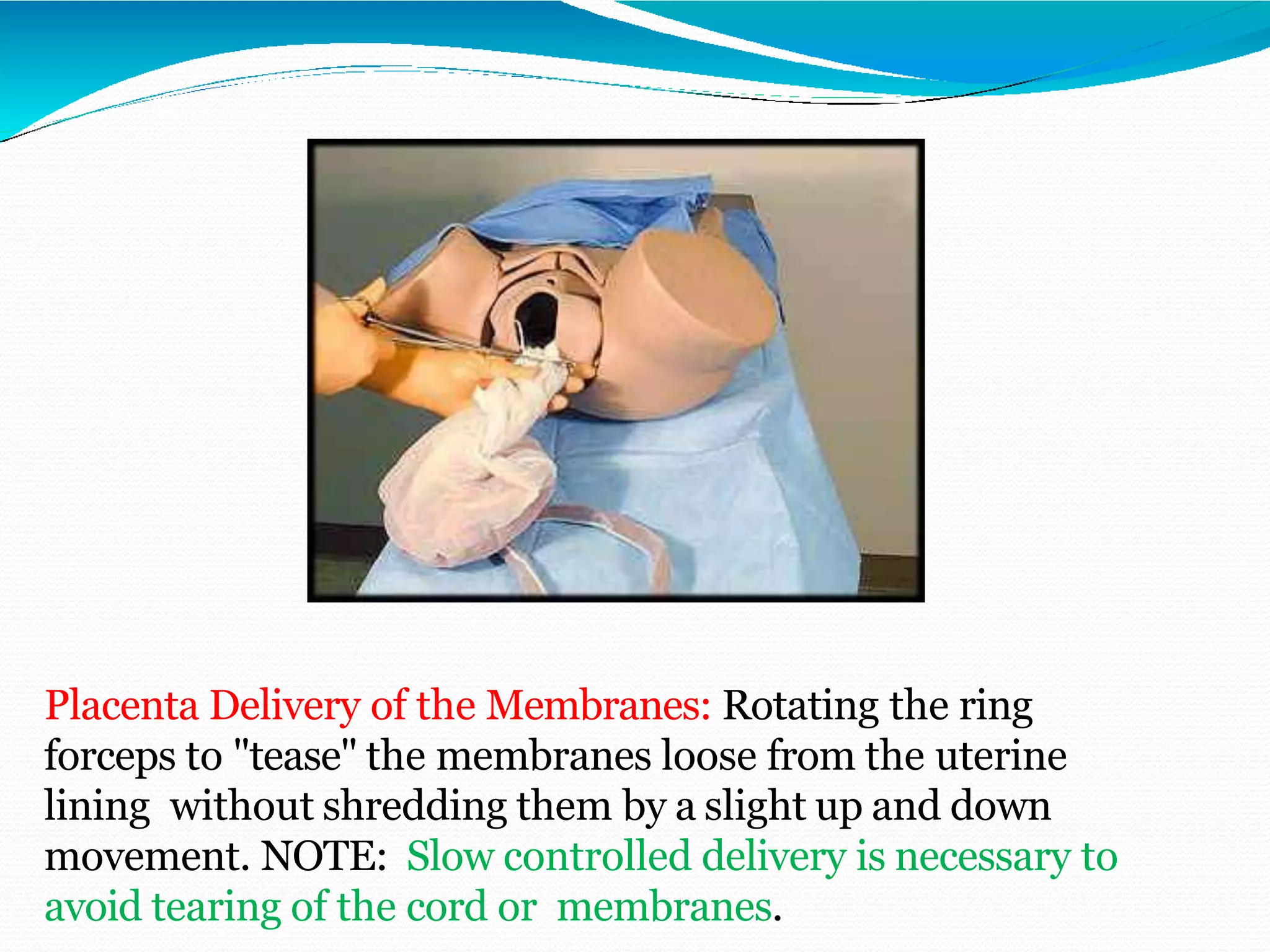
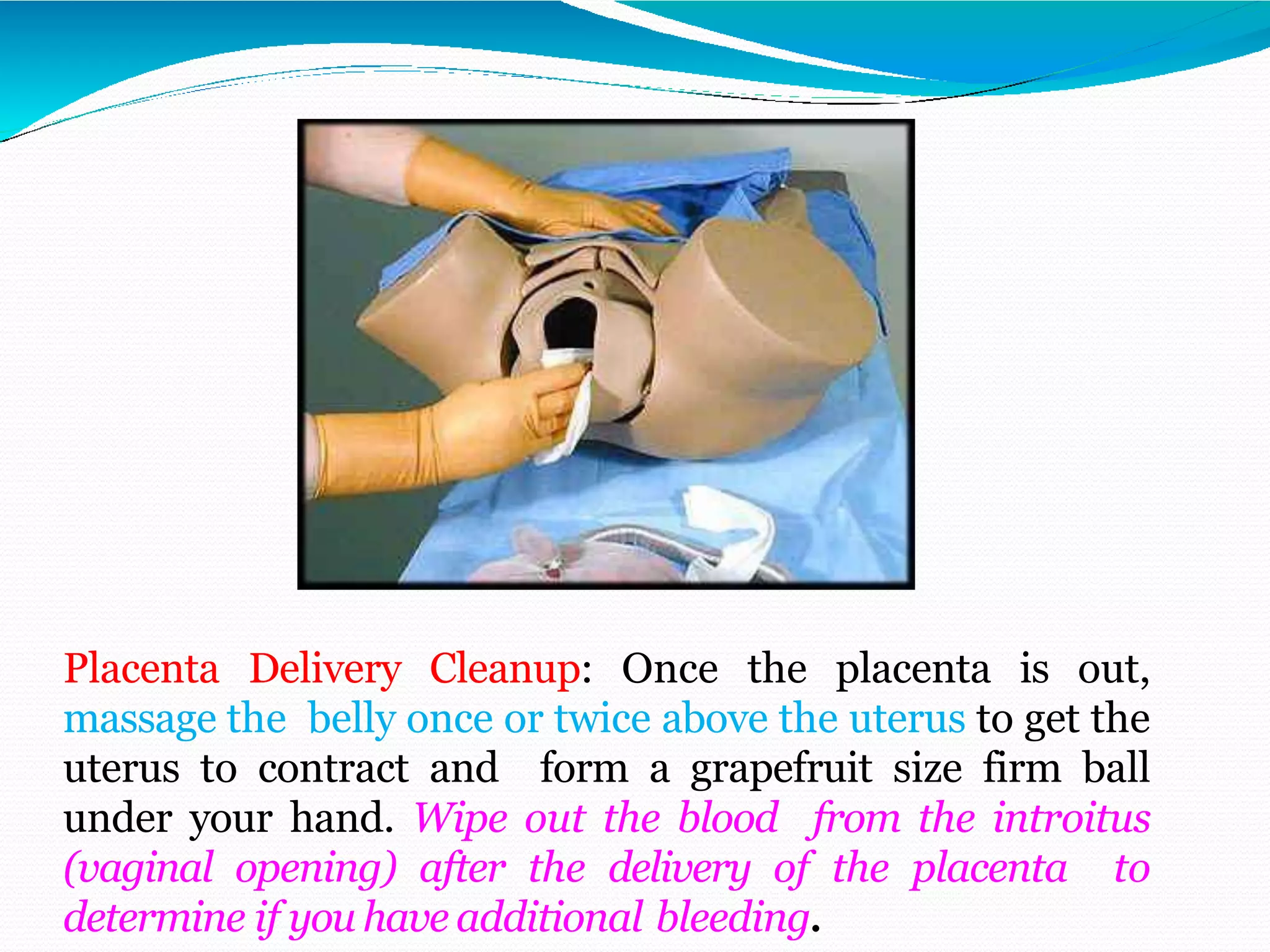
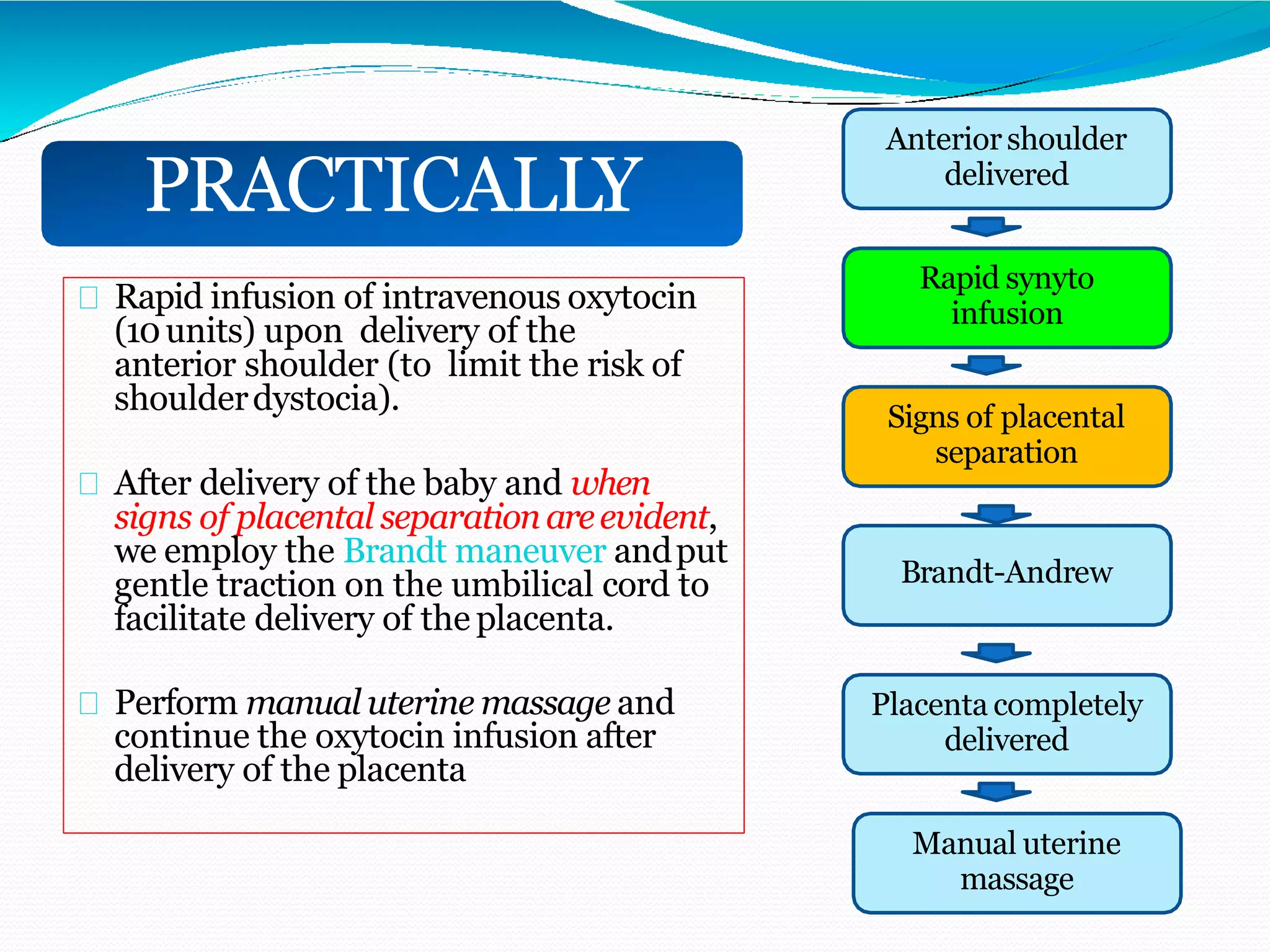
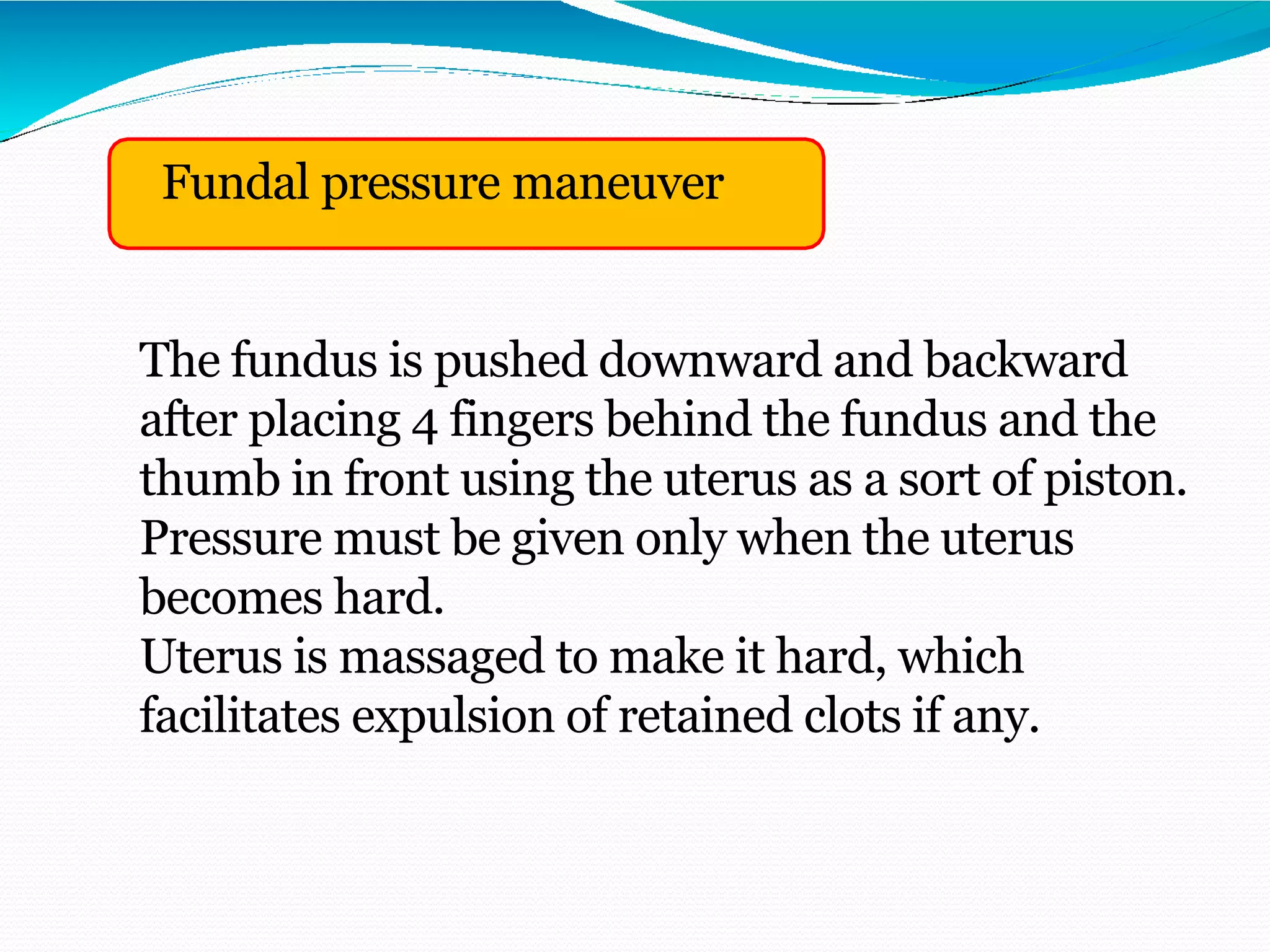
The third stage of labor involves the delivery of the placenta after birth of the baby. Active management with controlled cord traction and uterotonic drugs is recommended to prevent postpartum hemorrhage. After ensuring placental separation with signs like cord lengthening and uterine contraction, gentle traction is applied to the cord while massaging the uterus to deliver the placenta in a controlled manner. Rapid intravenous oxytocin is given after birth to aid placental separation and reduce bleeding risk.