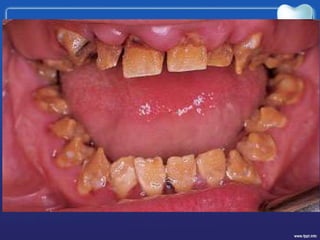
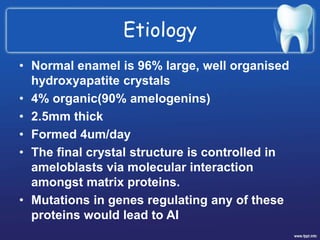
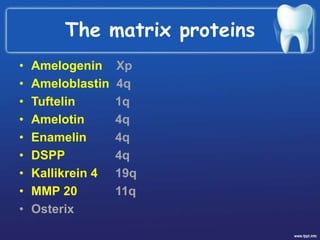
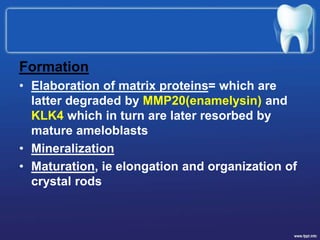
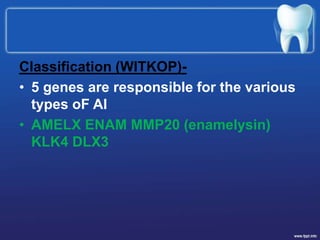
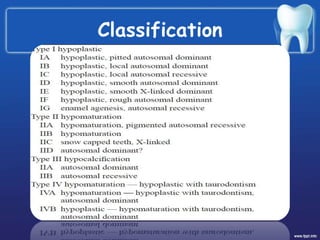
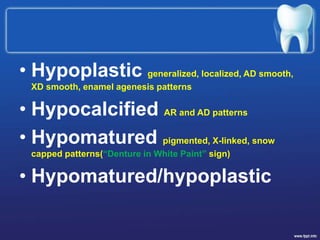
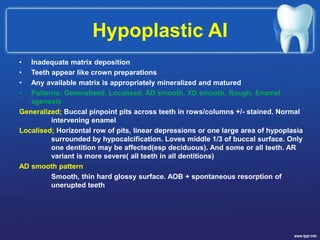
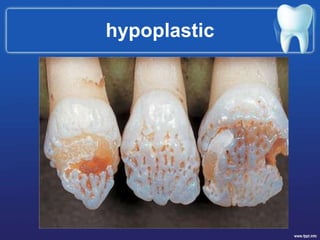
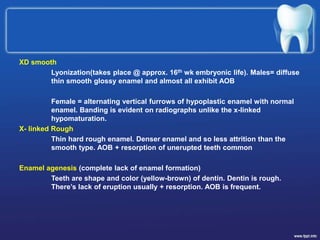
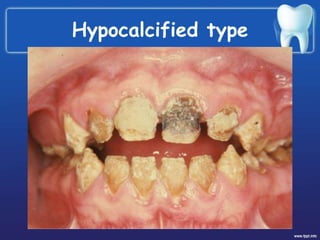
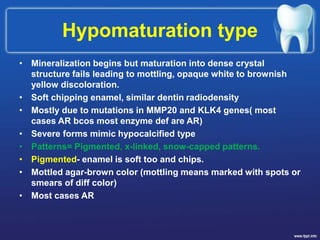
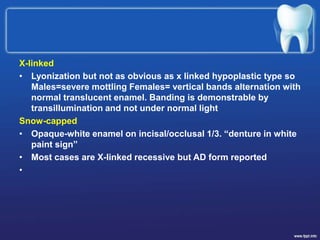
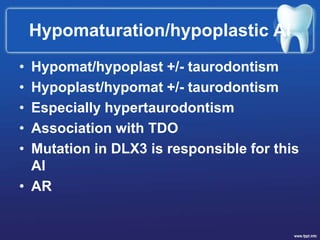
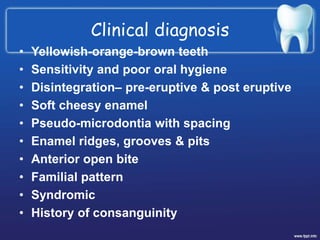
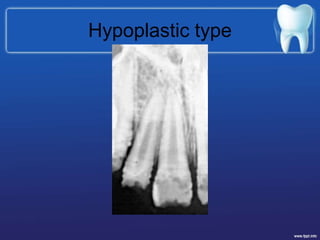
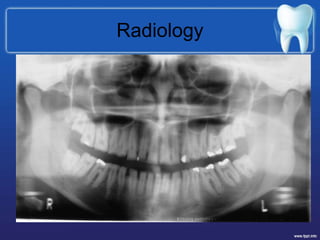
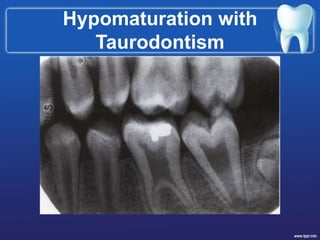
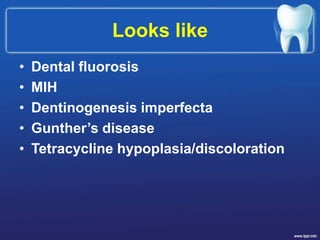
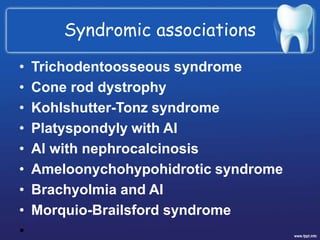
Amelogenesis Imperfecta is a condition affecting the development of dental enamel. It has several classifications depending on the specific enamel defect present, including hypoplastic (inadequate enamel), hypocalcified (no mineralization), and hypomaturation (failure of enamel to mature). The condition can be inherited in autosomal dominant, recessive, x-linked, or sporadic patterns. Diagnosis is based on family history, clinical examination showing discolored, sensitive teeth prone to disintegration, and radiographic findings of abnormal enamel appearance. It may occur alone or be associated with other systemic abnormalities in syndromes.