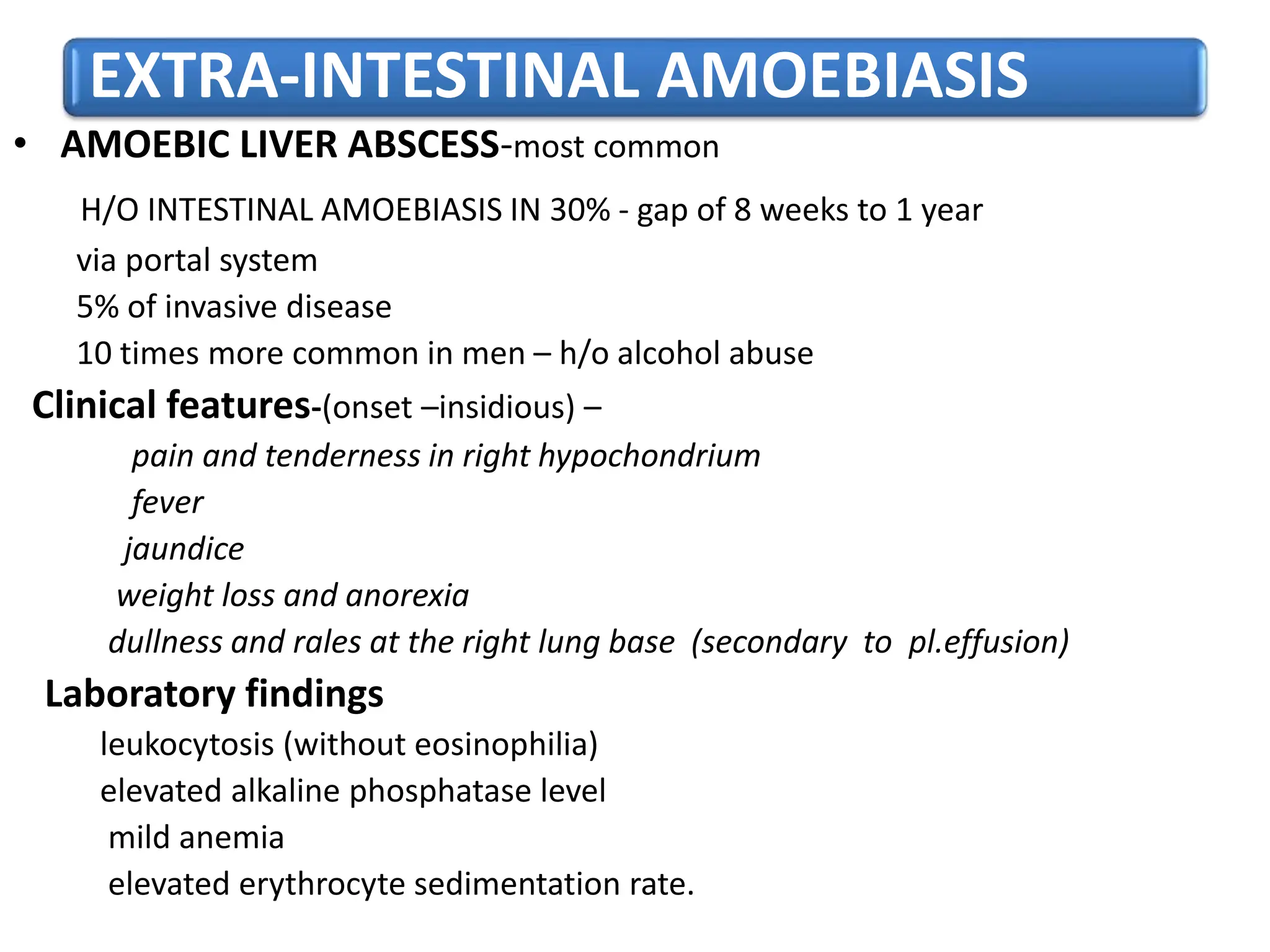
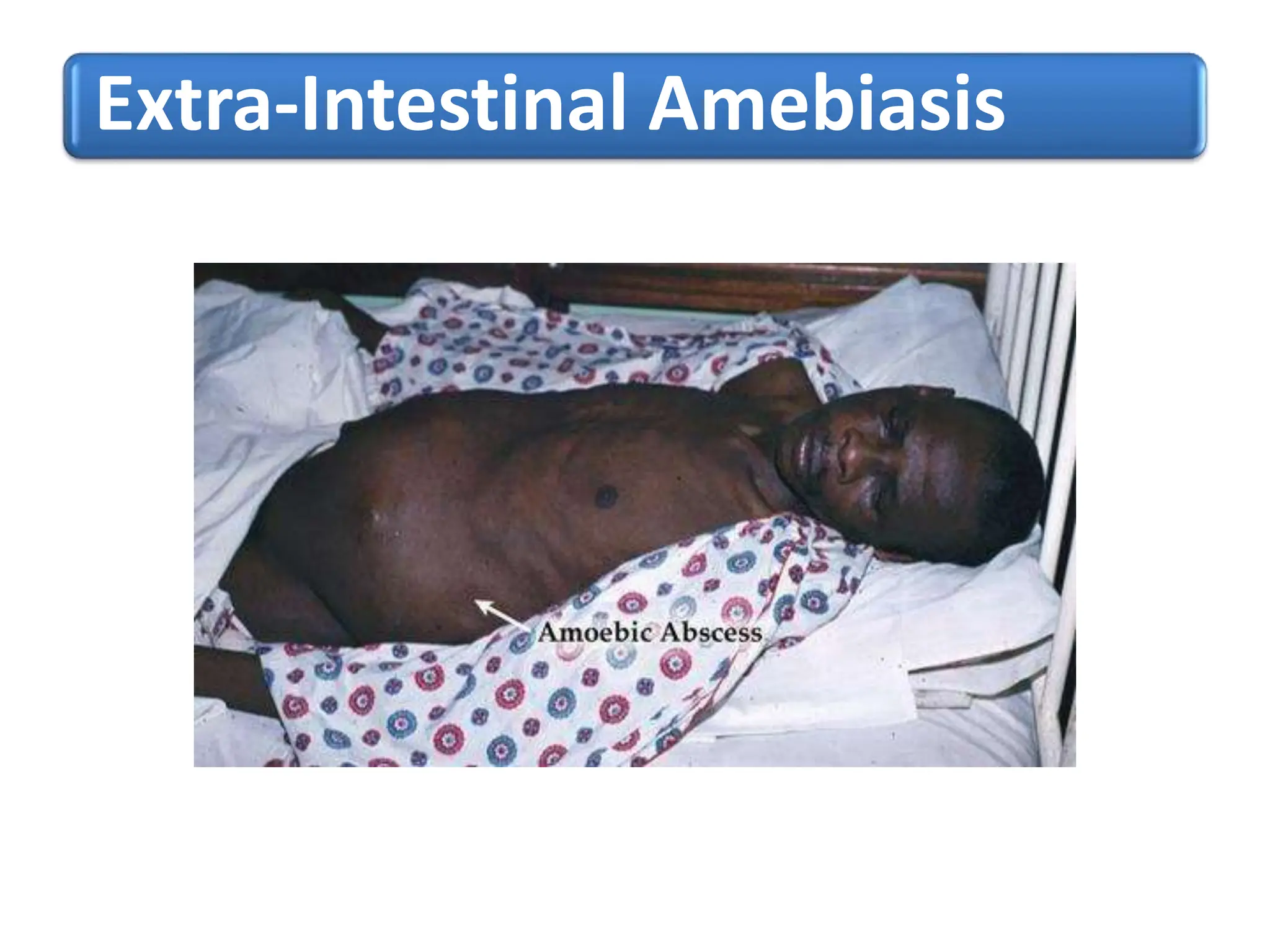
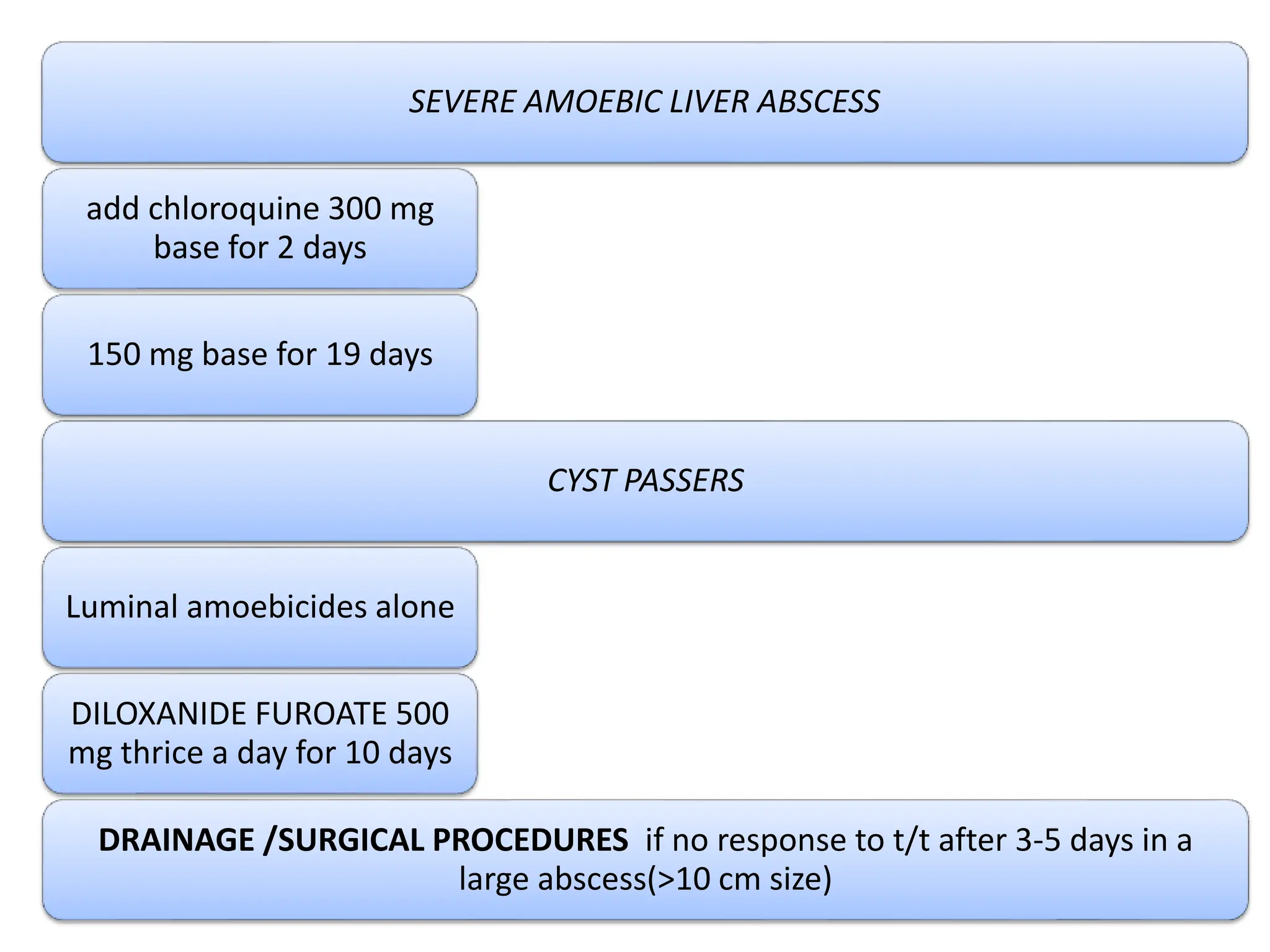
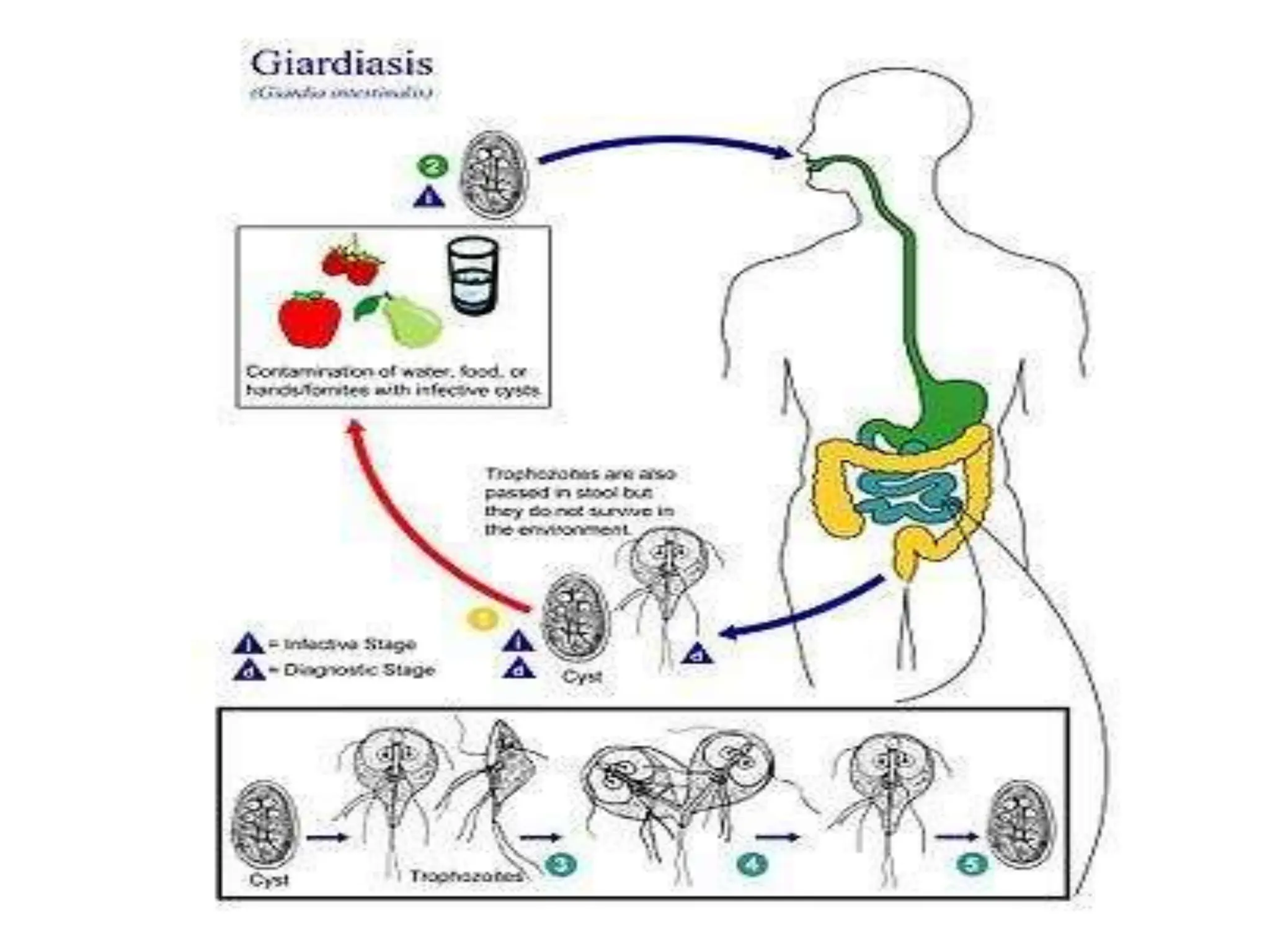
Amebiasis is an infection caused by Entamoeba histolytica, prevalent in developing countries with poor sanitary conditions. It can lead to severe intestinal and extra-intestinal complications, including amoebic dysentery and liver abscesses, and is diagnosed through stool examinations and serological tests. Treatment involves anti-amoebic medications such as metronidazole and luminal amoebicides, with prevention focused on maintaining good hygiene and proper water treatment.