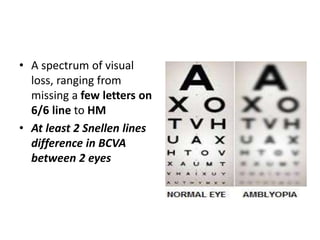
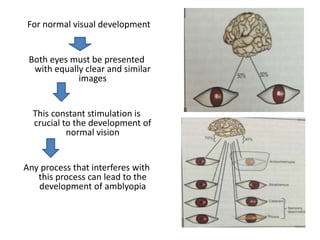
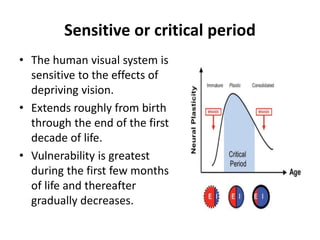
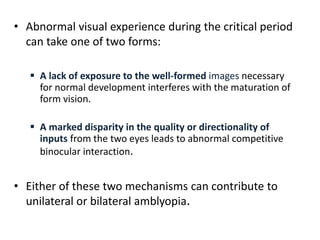
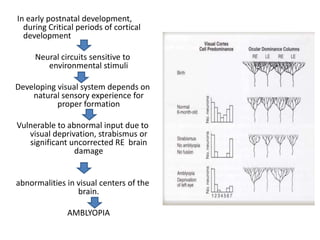
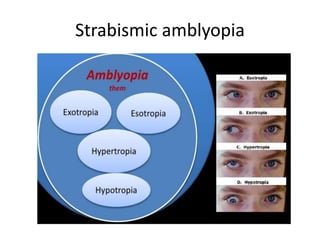
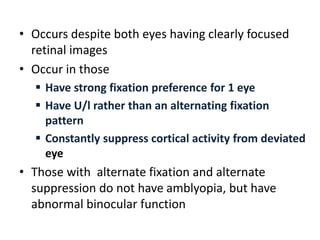
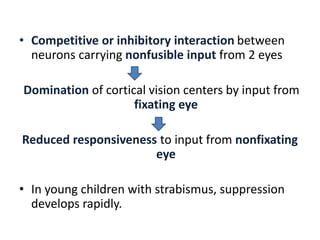
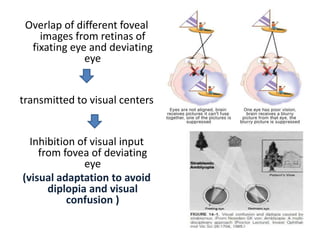
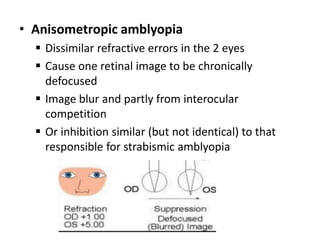
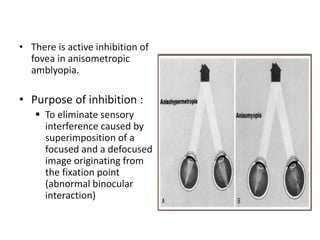
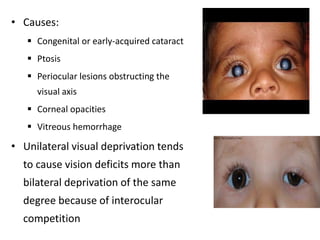
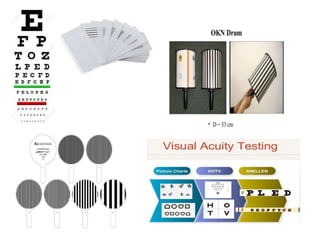
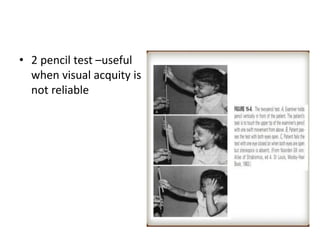
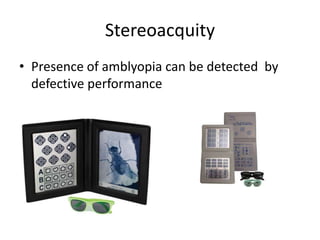
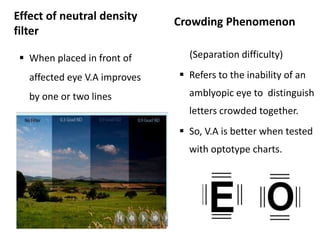
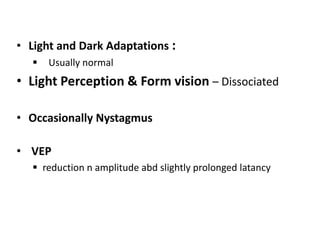
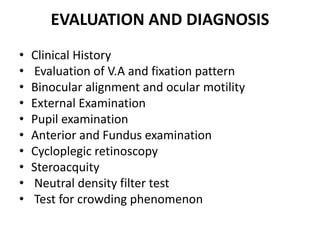
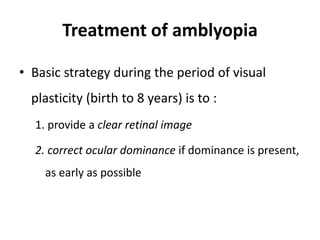
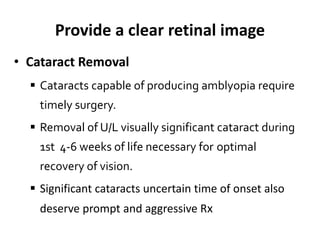
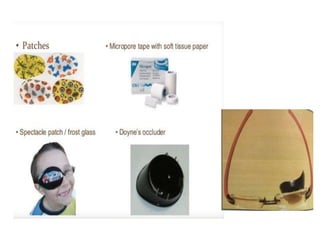
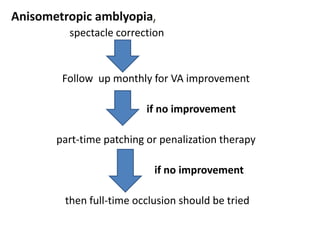
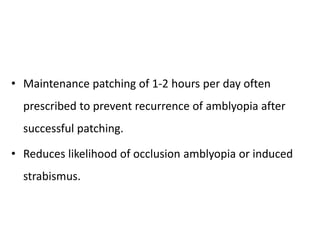
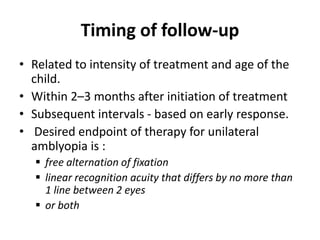
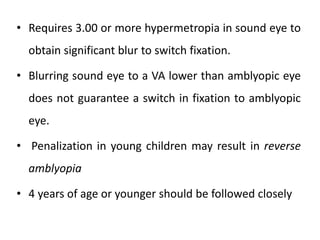
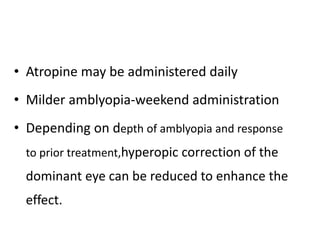
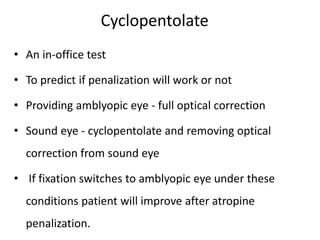
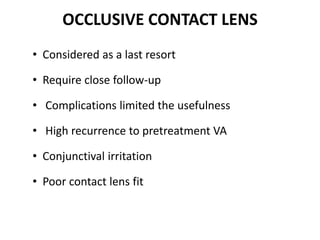
This document provides an overview of amblyopia, including its definition, pathophysiology, classification, clinical characteristics, evaluation, diagnosis, and treatment. Amblyopia is reduced best-corrected visual acuity that cannot be attributed to a structural abnormality and develops due to abnormal visual experience during the visual system's critical period of development early in life. It is classified based on etiology, such as strabismic, refractive, or deprivation amblyopia. Treatment focuses on providing a clear retinal image and correcting ocular dominance through refractive correction and occlusion or penalization therapy, with the goal of improving visual acuity before the end of the critical period.