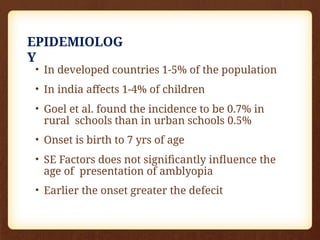
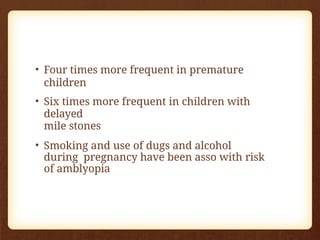
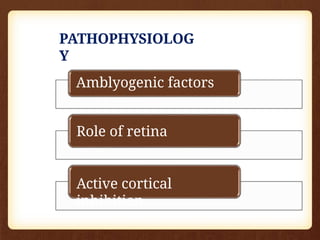
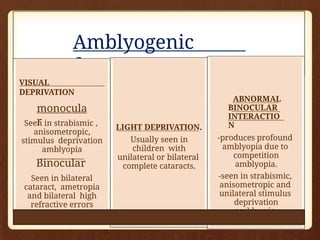
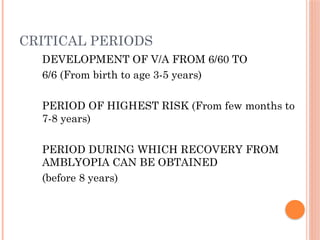
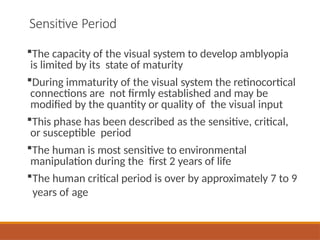
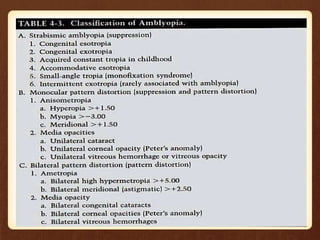
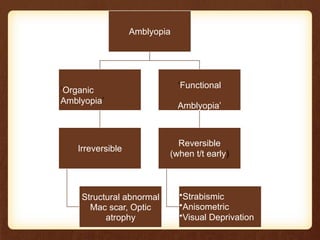
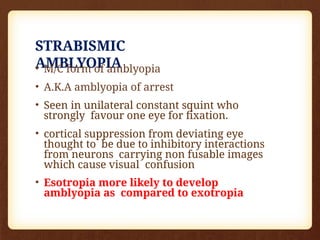
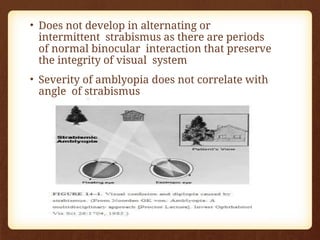
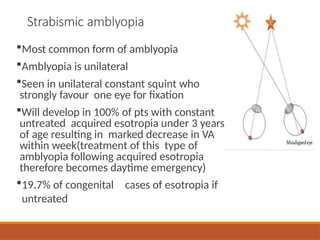
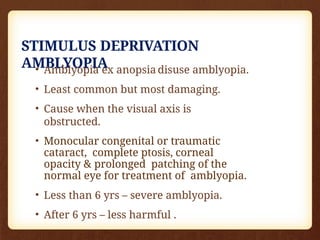
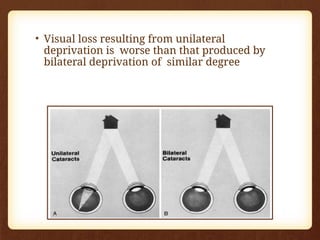
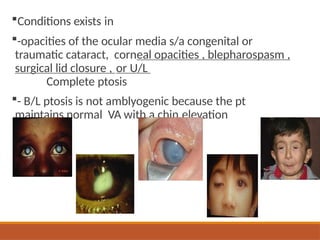
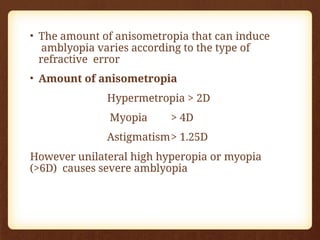
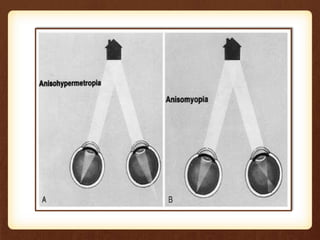
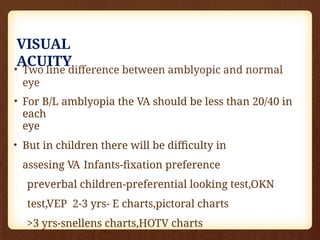
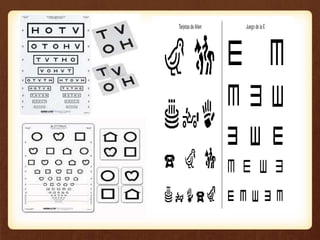
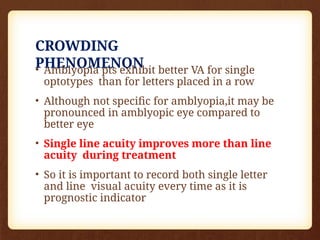
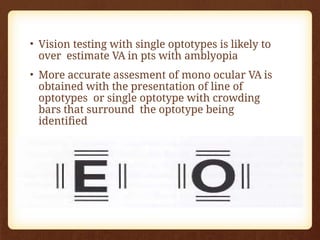
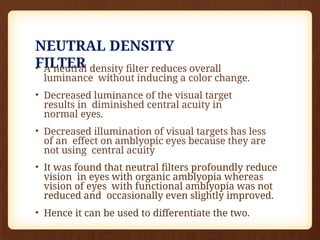
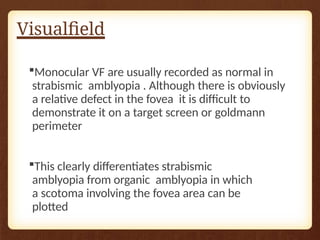
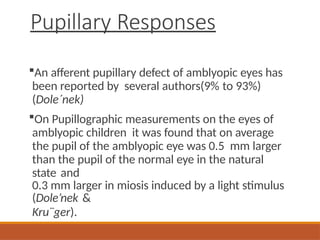
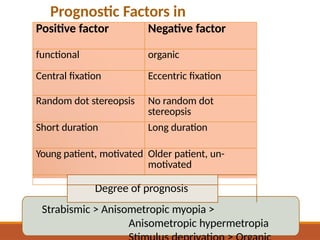
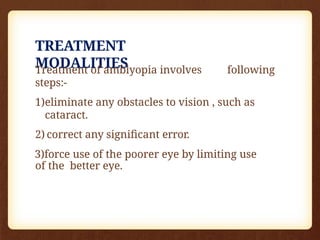
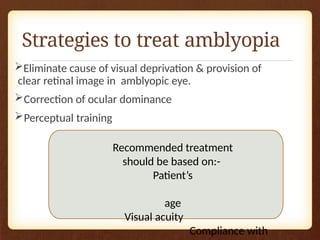
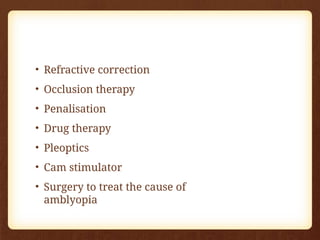
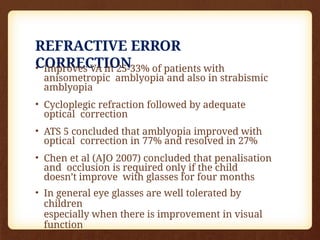
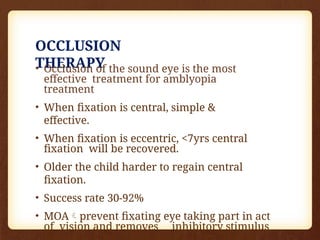
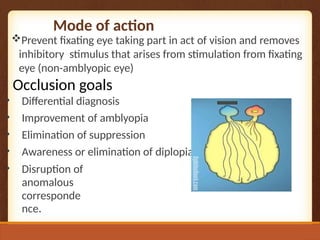
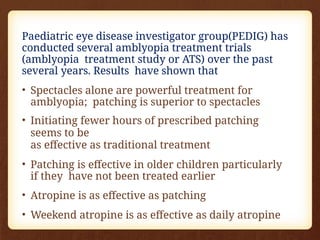
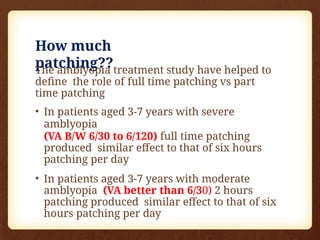
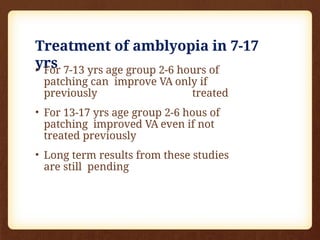
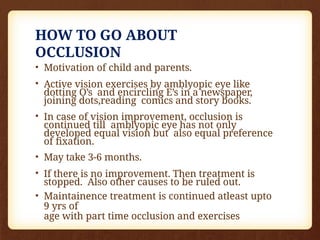
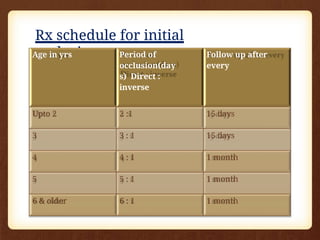
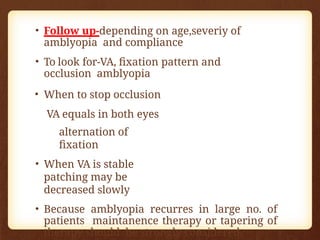
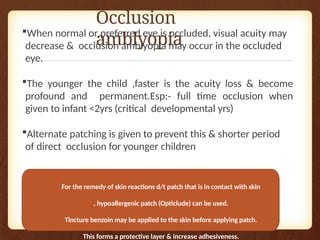
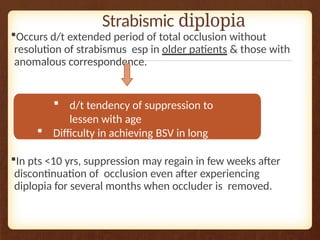
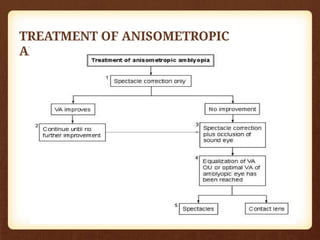
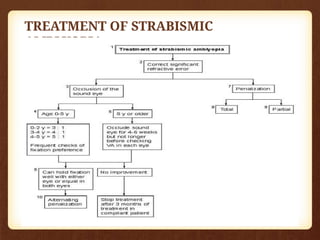
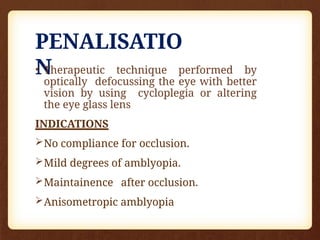
Amblyopia, or lazy eye, is a vision disorder characterized by reduced visual acuity in one or both eyes that persists even after correcting refractive errors. This condition affects a significant percentage of children across various demographics, with its incidence related to factors such as age, cultural background, and prenatal exposure to harmful substances. Various types of amblyopia exist, including strabismic, stimulus deprivation, and anisometropic amblyopia, each requiring different treatment approaches to improve visual outcomes.