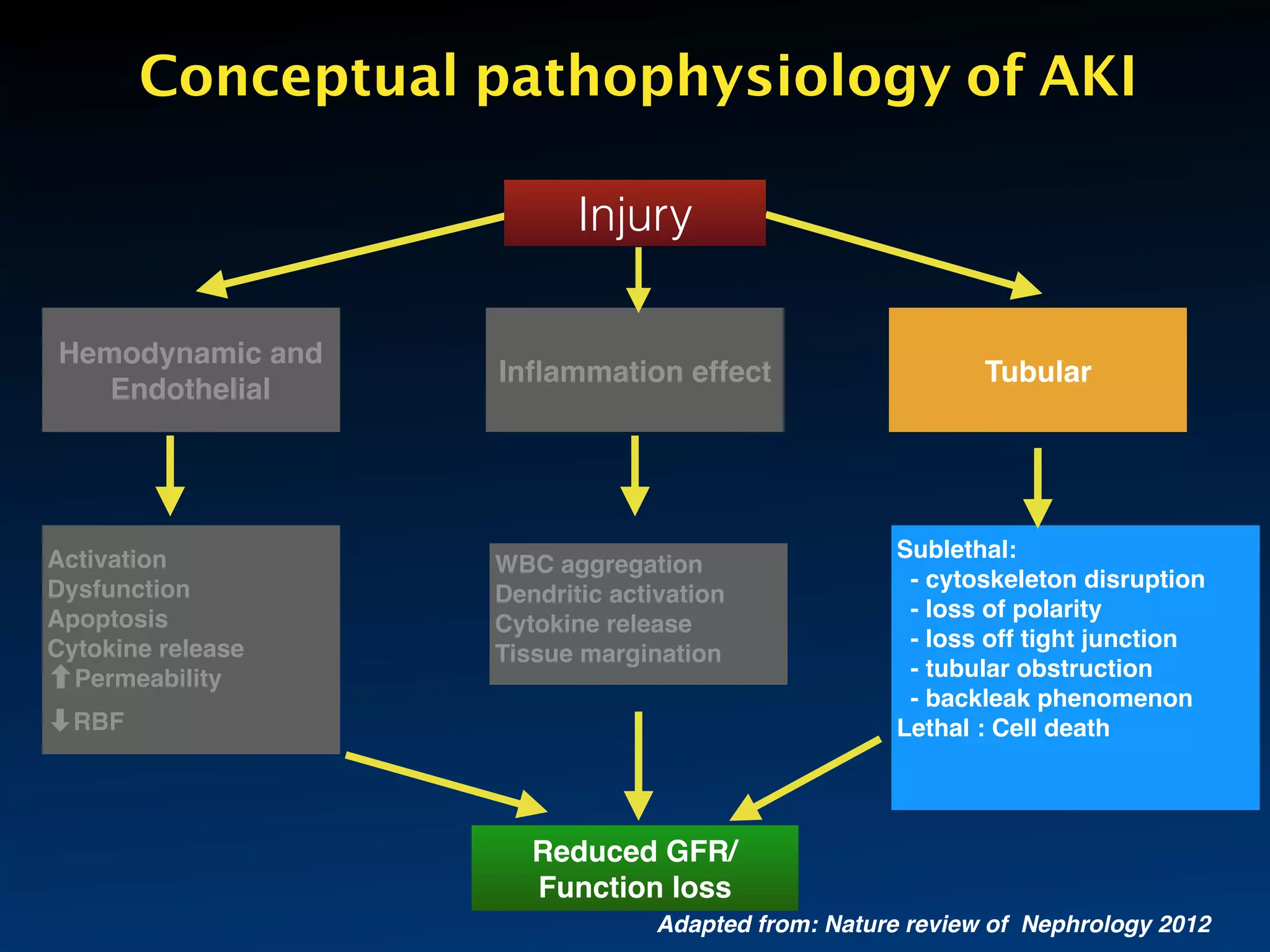
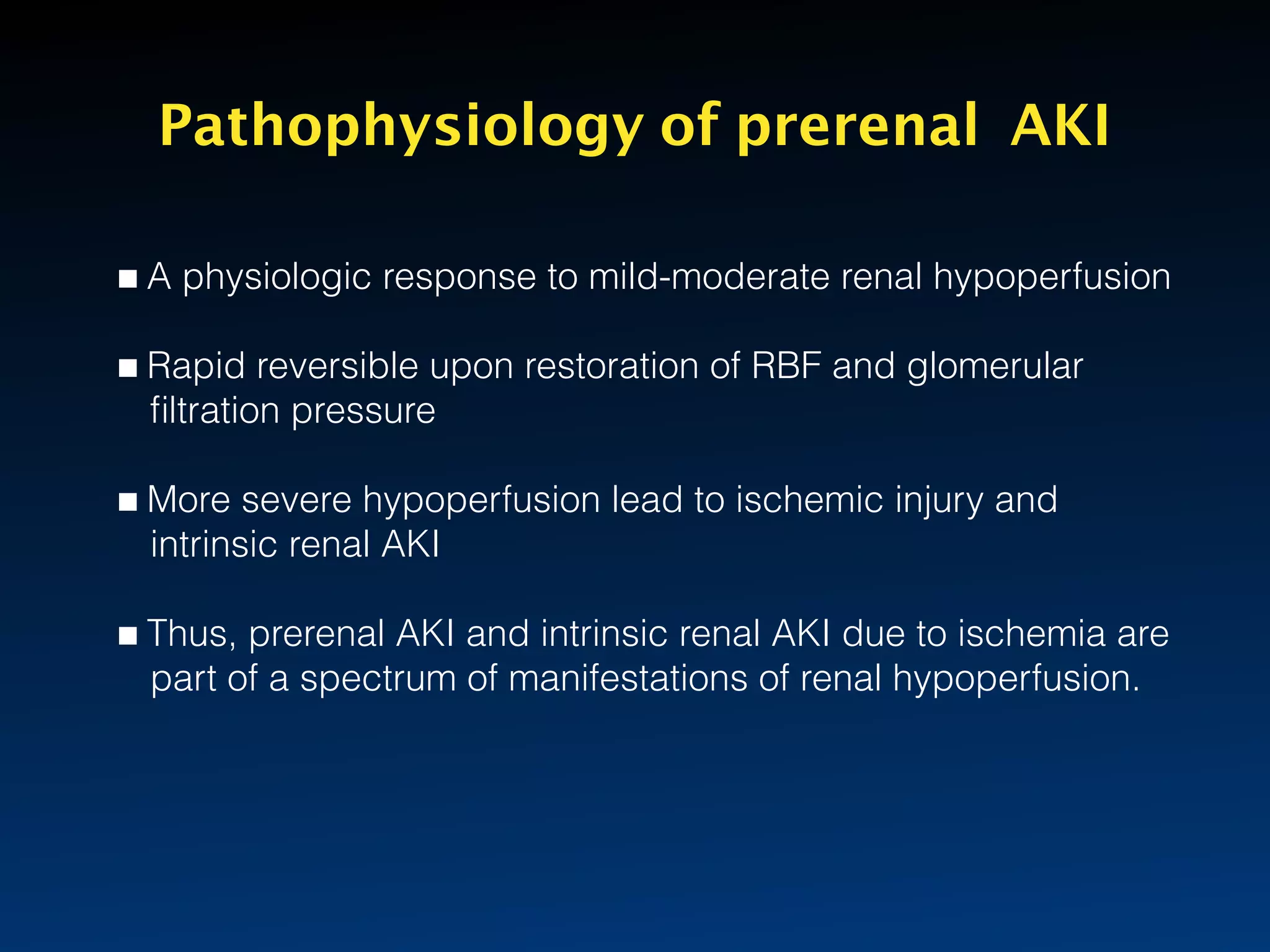
This document discusses the pathophysiology of acute kidney injury (AKI). It covers pre-renal, post-renal and intrinsic renal AKI. For intrinsic renal AKI, it focuses on acute tubular necrosis (ATN). It describes the hemodynamic changes, endothelial dysfunction, inflammatory response and tubular injury that occur in ATN. Hemodynamic changes like renal hypoperfusion can cause ischemia. This results in endothelial activation, leukocyte recruitment and coagulation changes. Tubular injury involves loss of polarity, cytoskeleton disruption and cell death via necrosis or apoptosis. The document provides details on the molecular mechanisms and pathways involved in each step of the pathophysiological process of ATN.




























![Key Inflammatory response after IRI
• Initiated by endothelial dysfunction with
leukocyte extravasation
• Macrophage release of proinflammatory
cytokines (TNF- 𝛼, IL-8,IL-1)
• Chemotactic cytokines (e.g., monocyte
chemoattractant protein-1 [MCP-1] IL-8, RANTES)
• Powerful recruits other inflammatory cells and
complement activation](https://image.slidesharecdn.com/akipathophysiologychaken-160821032827/75/AKI-pathophysiology-chaken-maniyan-30-2048.jpg)