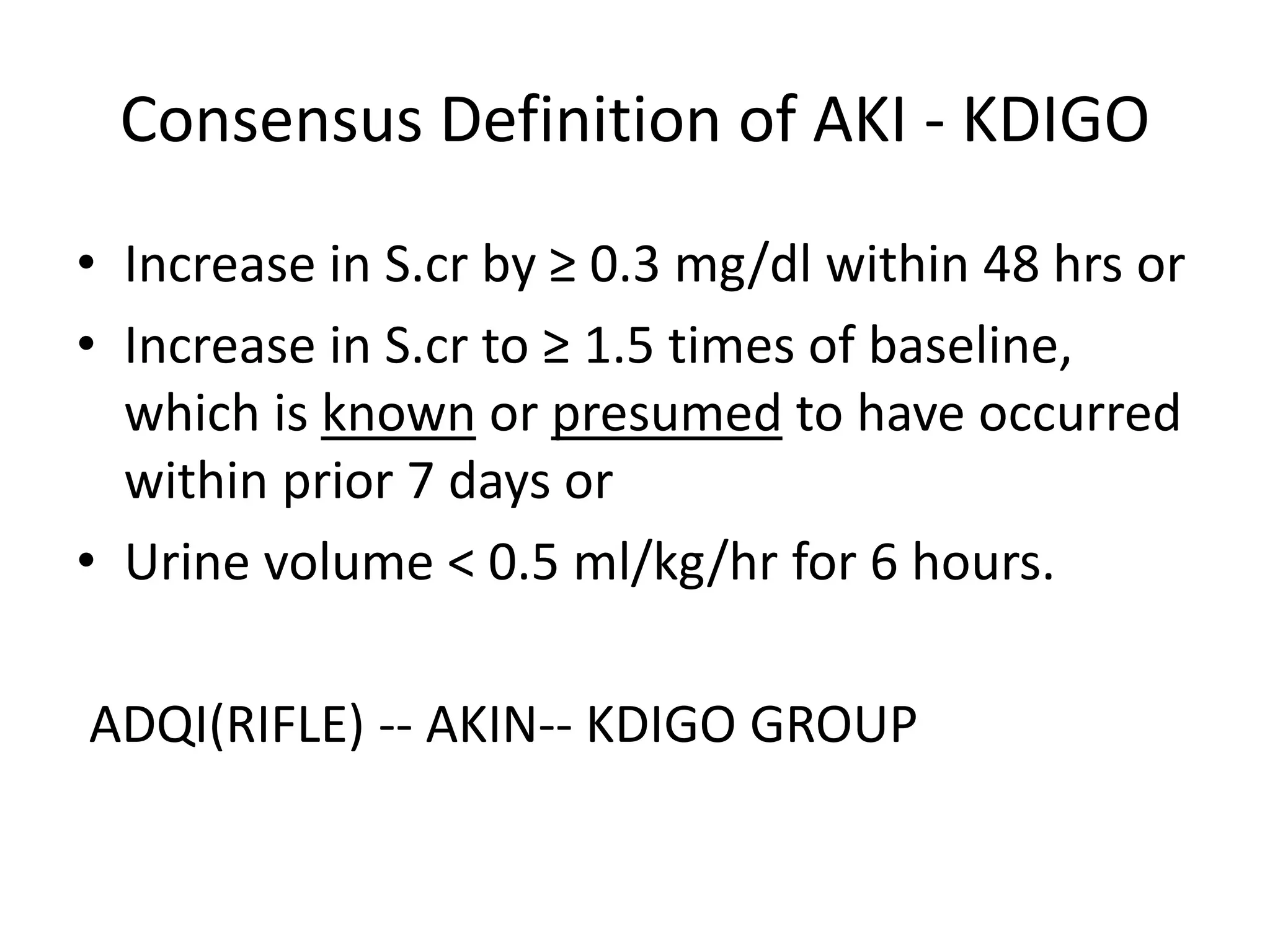
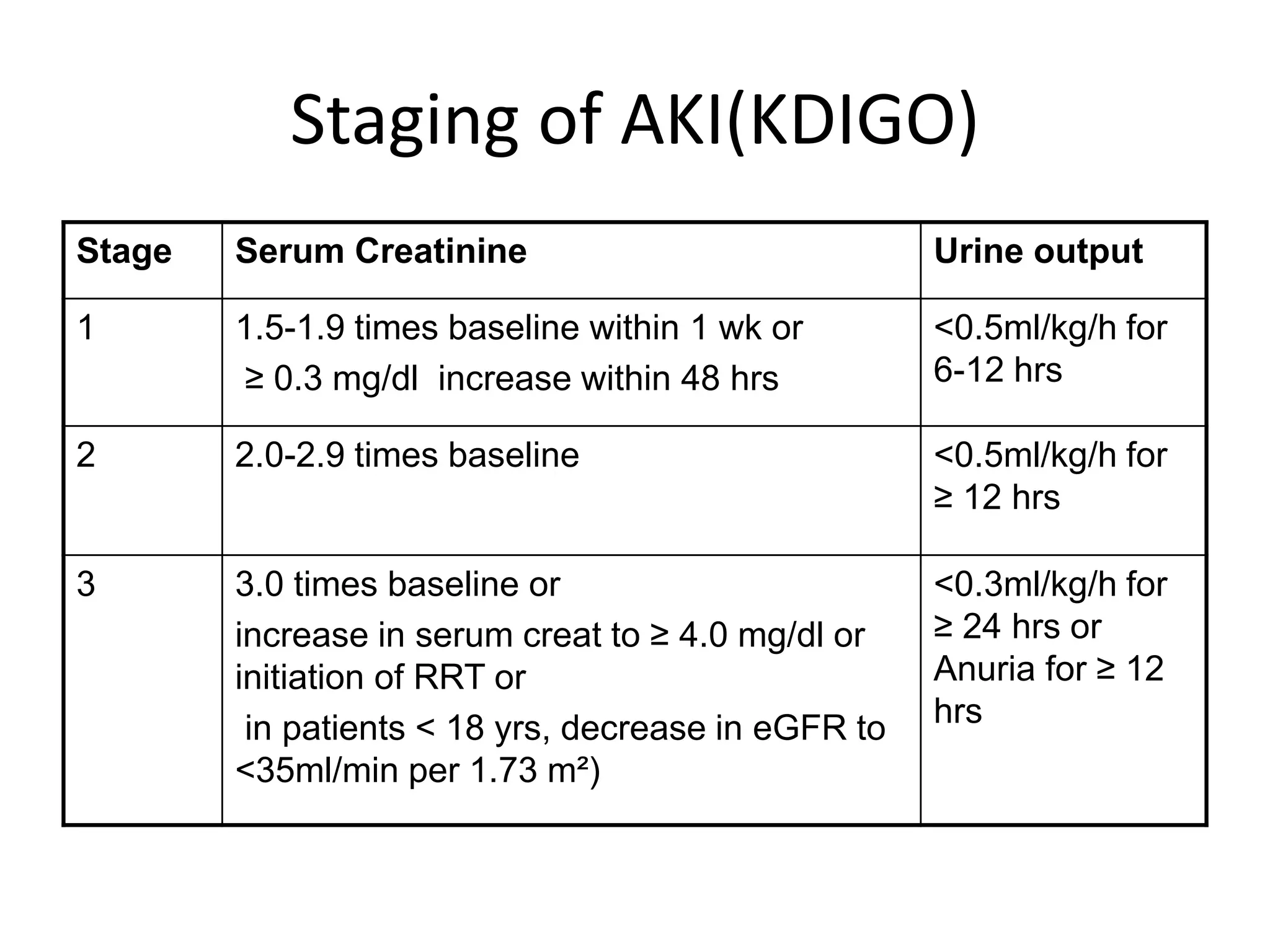
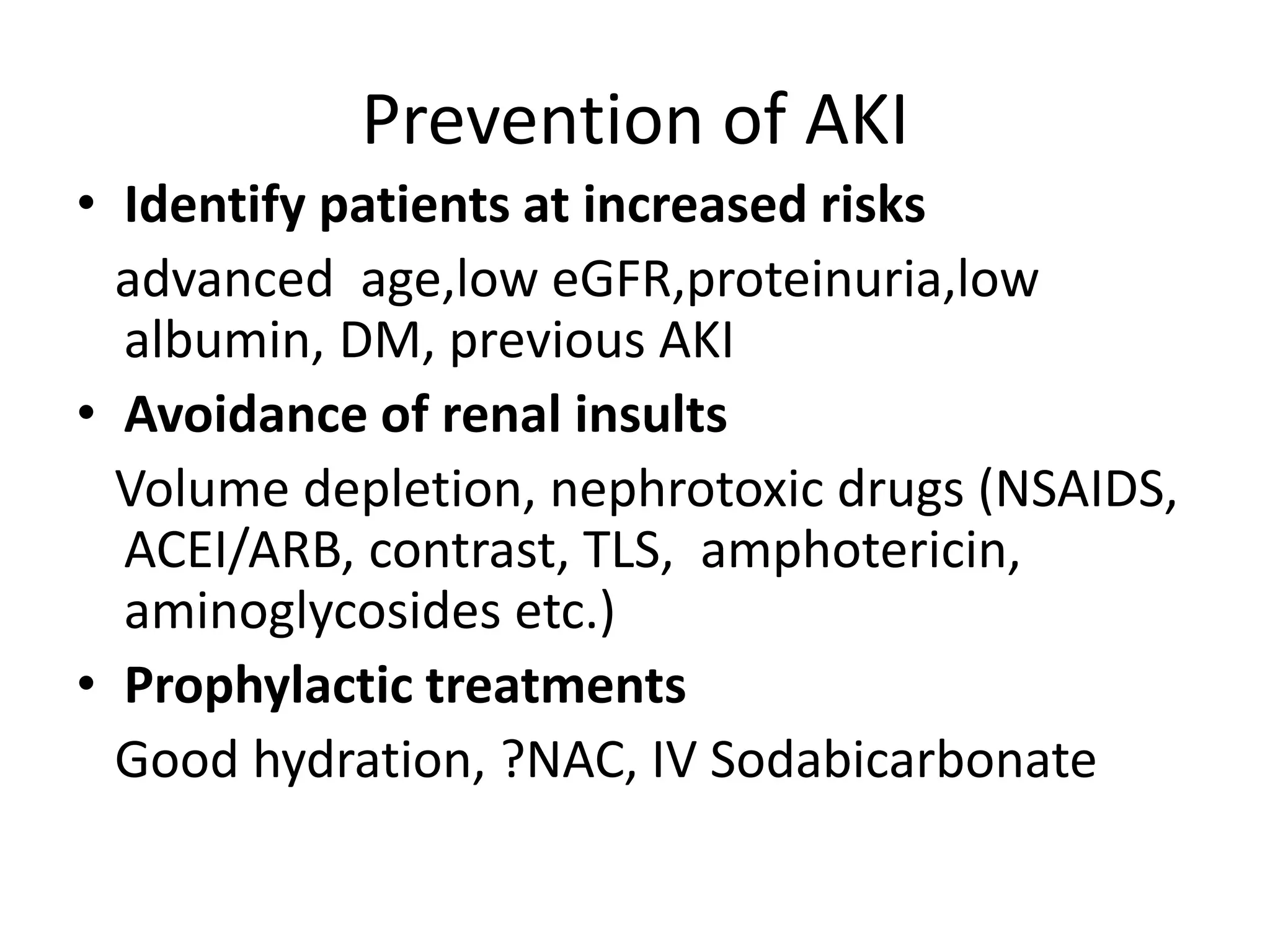
Acute Kidney Injury (AKI) is characterized by a rapid and sustained decrease in renal function, with significant morbidity and mortality associated with it. Key aspects include its epidemiology, causes, and the emerging importance of biomarkers for early diagnosis. Management involves identifying causes, staging severity, and treating complications, while recent discussions highlight the lack of consensus on the most effective renal replacement therapy methods.