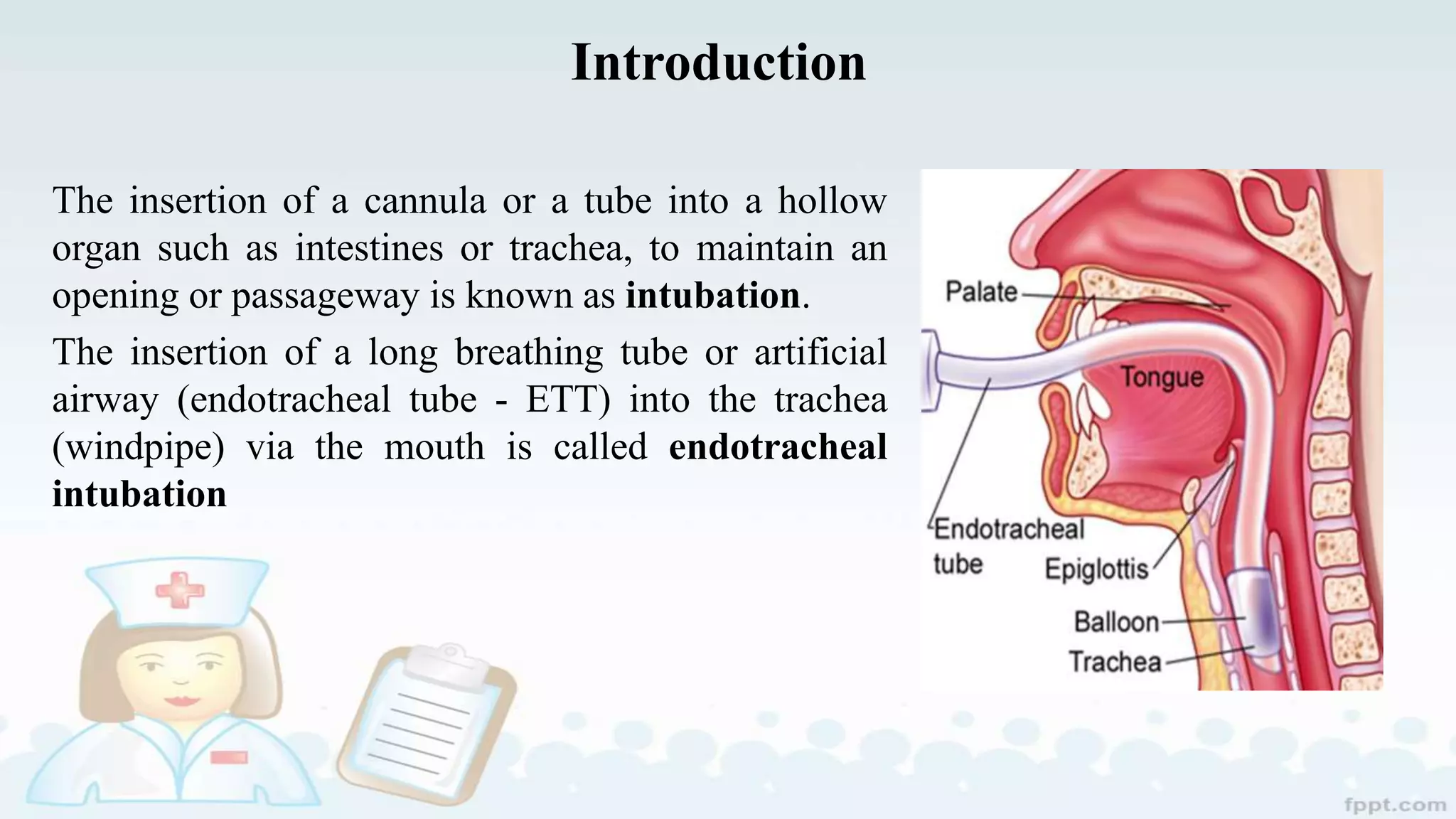
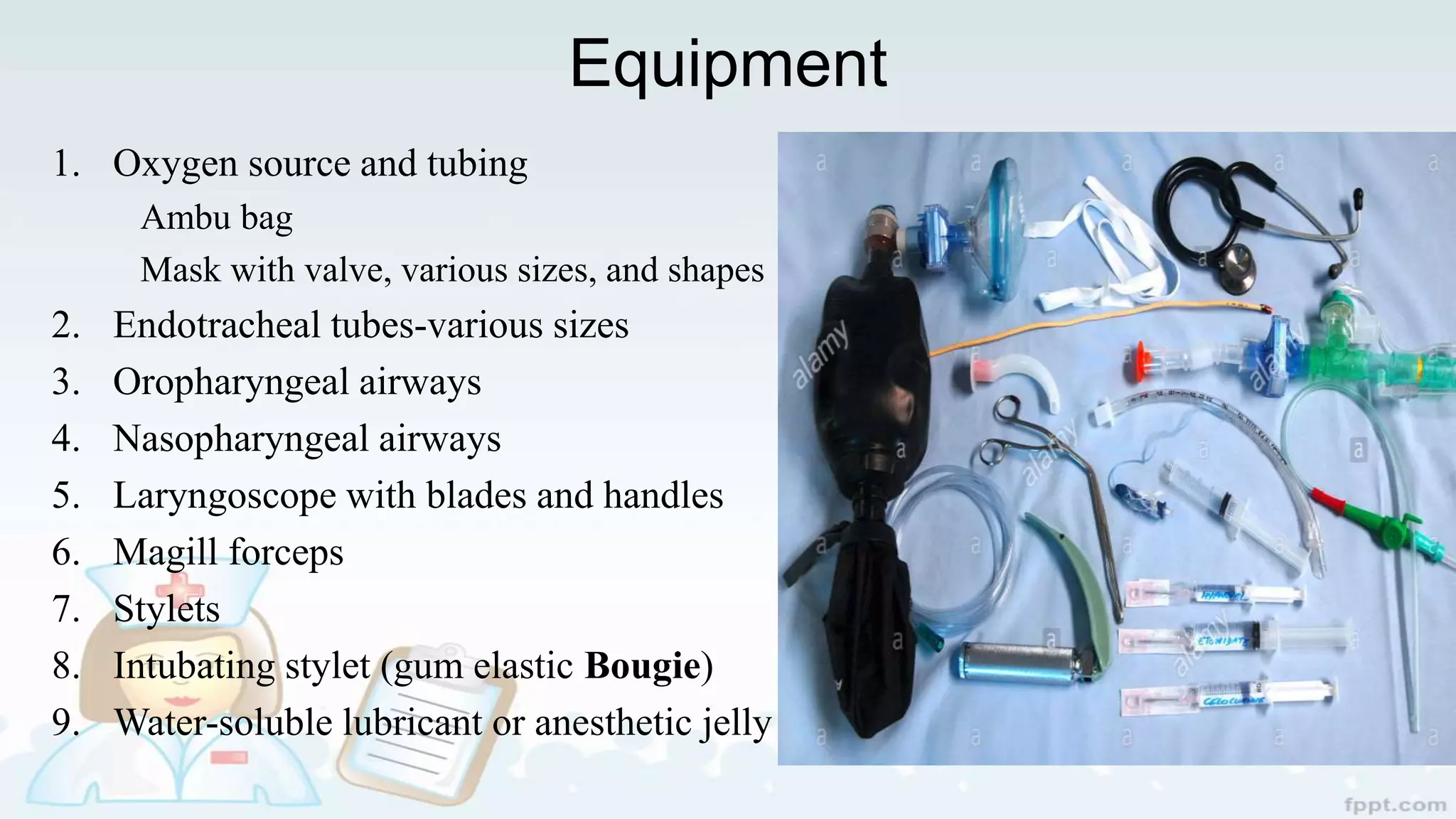
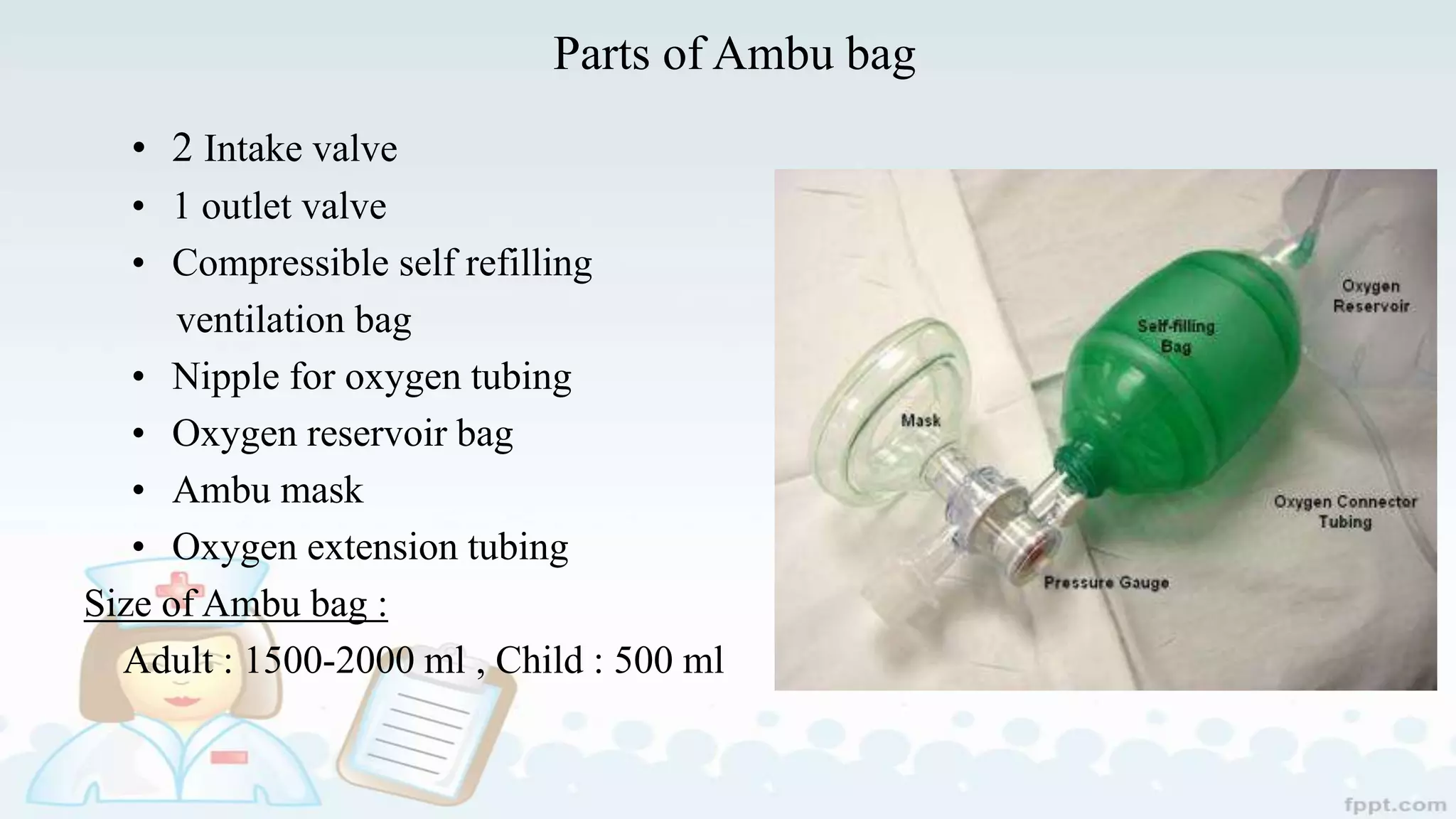
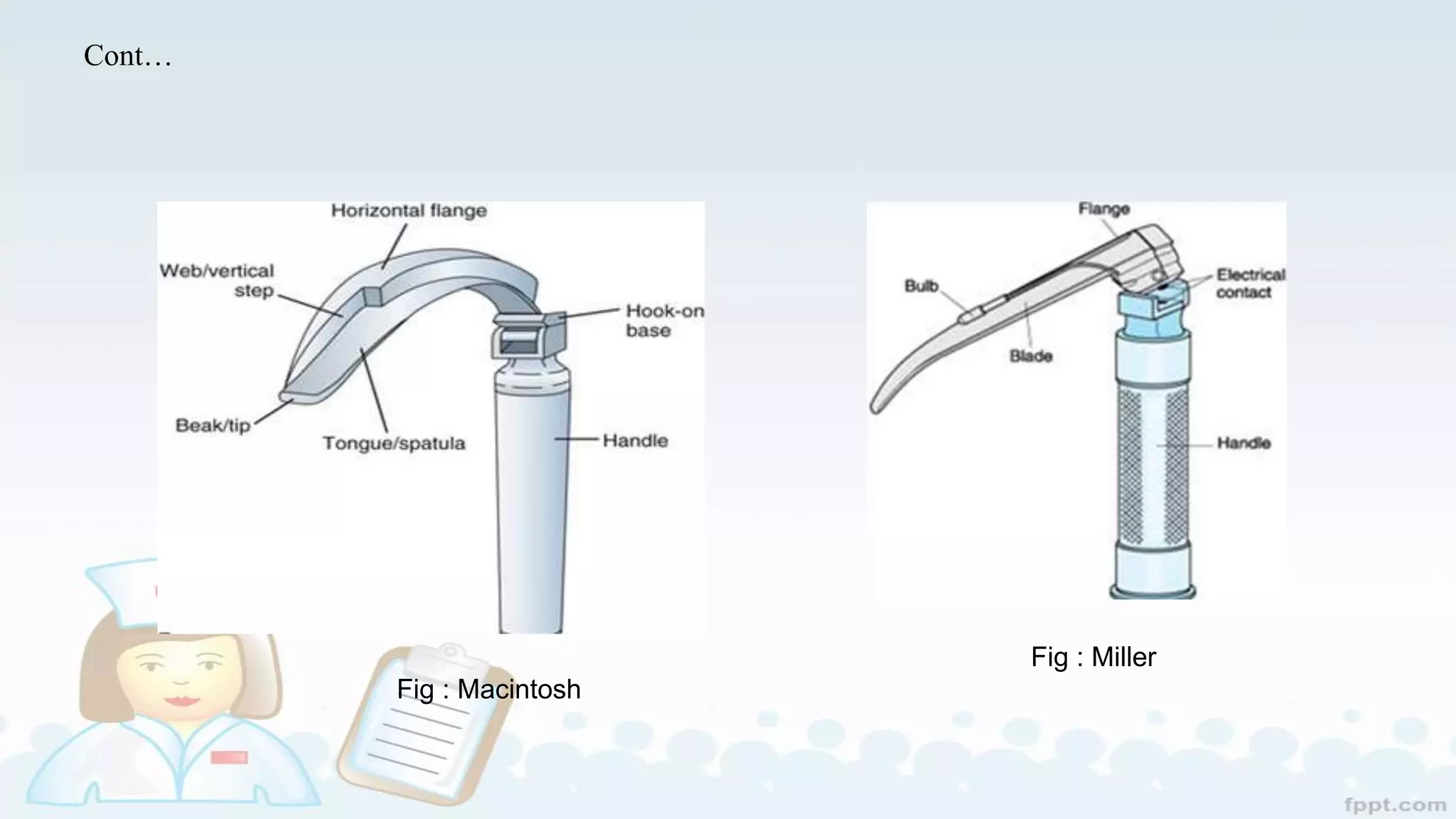
The document provides an extensive overview of endotracheal intubation, including procedures, advantages, and disadvantages of oral versus nasal intubation. It details equipment necessities, complications, and techniques for intubation, as well as post-intubation care and extubation procedures. The content is designed for nursing students and professionals involved in critical care scenarios.