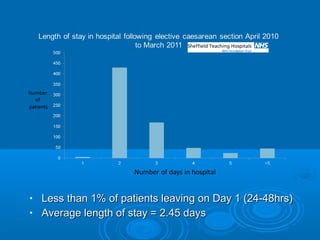
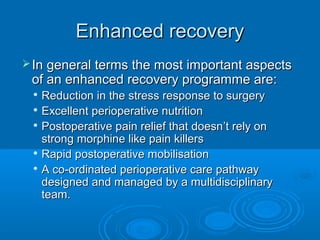
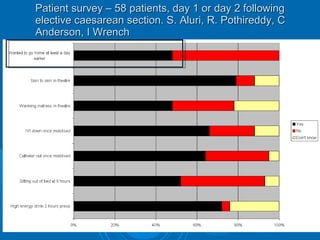
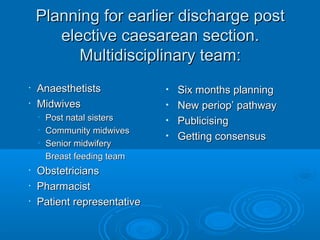
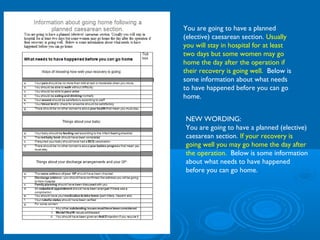
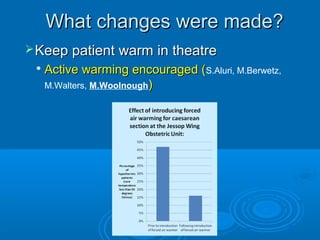
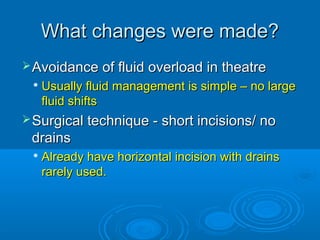
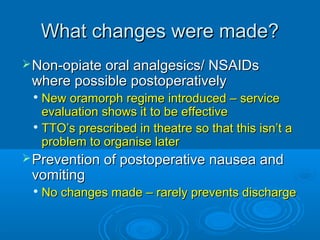
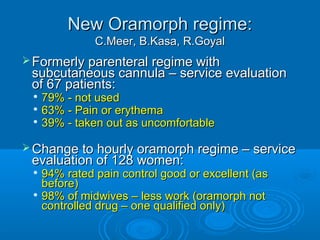
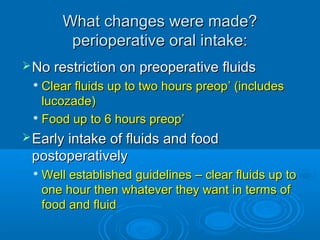
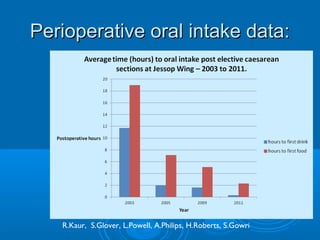
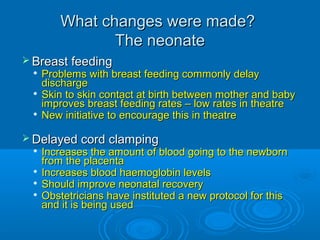
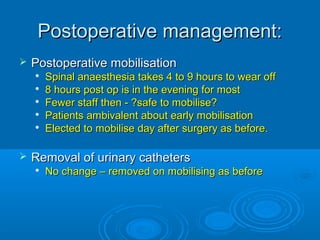
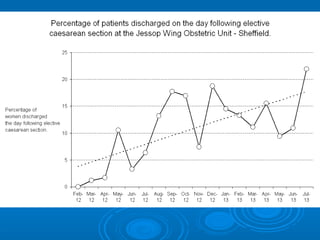
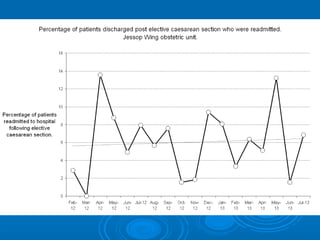
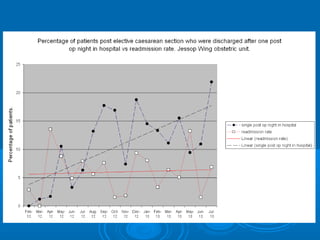
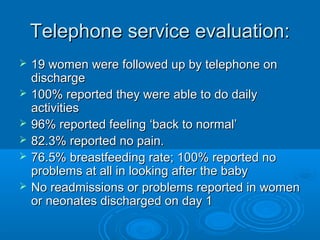
The document discusses the implementation of an enhanced recovery care pathway for elective caesarean sections, which has led to a significant increase in the percentage of patients being discharged on day one, from less than 1% to 15-20%. Key changes included preoperative counseling, carbohydrate loading, non-opiate analgesics, and improved postoperative care, all contributing to good patient outcomes without increasing readmission rates. Future developments aim to apply these strategies to emergency caesarean sections and enhance practices such as skin-to-skin contact and delayed cord clamping.