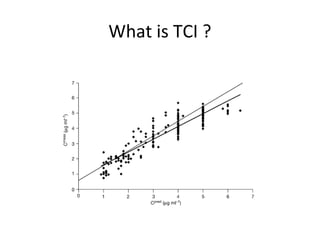
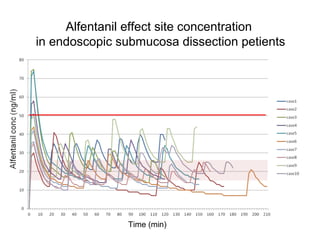
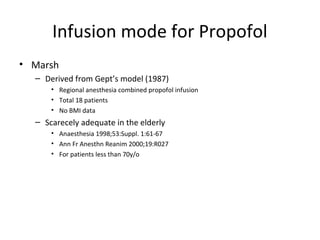
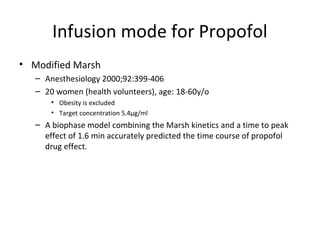
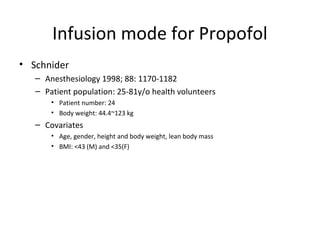
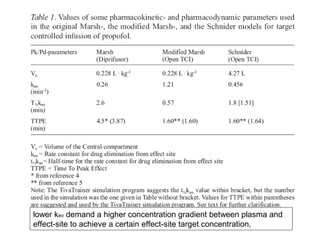
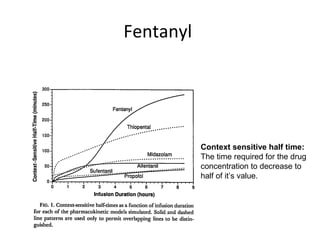
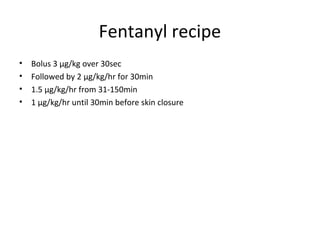
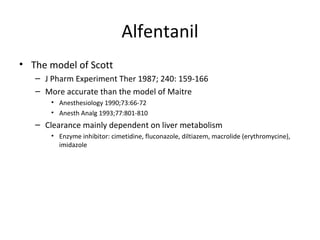
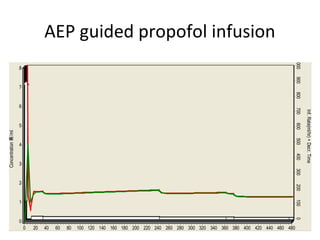
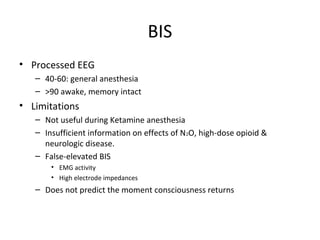
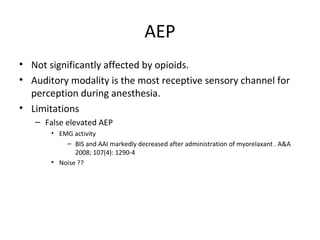
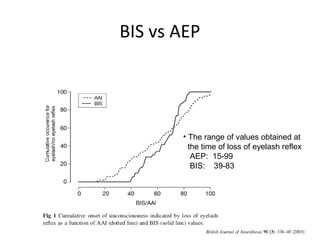
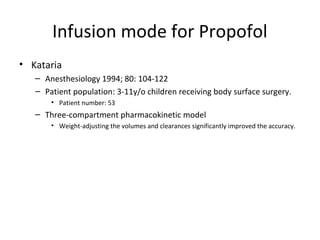
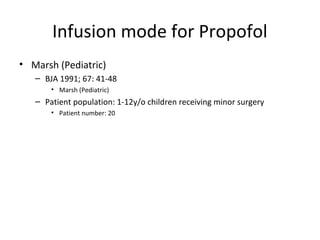
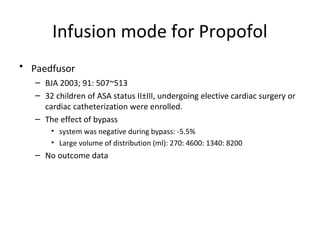
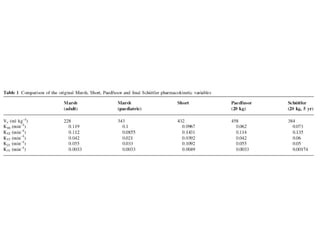
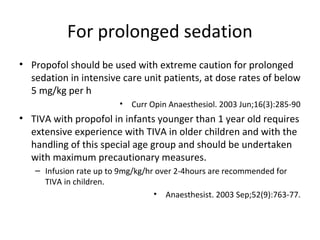
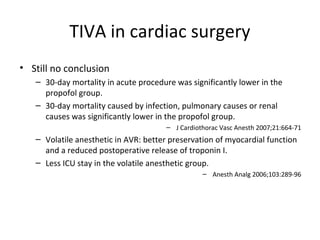
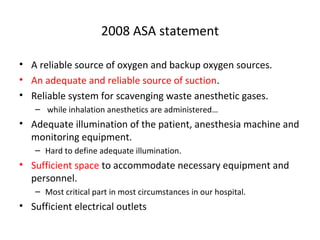
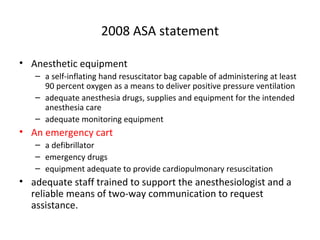
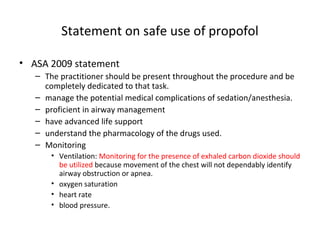
Total intravenous anesthesia (TIVA) and target controlled infusion (TCI) were discussed. TCI uses infusion models like Marsh and Schnider to calculate the target effect-site concentration of drugs like propofol and opioids to achieve anesthesia. Monitoring anesthetic depth with tools like BIS or AEP is recommended to optimize drug delivery and avoid overdose. While TIVA is commonly used in adults, data in pediatrics is still limited especially for infants, and propofol requires caution for prolonged sedation in ICU. No consensus was reached on whether volatile or intravenous agents lead to better outcomes in cardiac surgery. Office-based anesthesia requires adequate monitoring, emergency equipment, and staff training for patient safety.