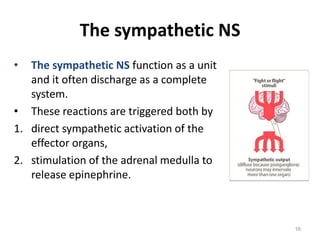
The document provides an overview of the autonomic nervous system and drugs that affect it. It discusses how the autonomic nervous system is responsible for involuntary bodily functions and is divided into the sympathetic and parasympathetic divisions. Drugs that affect the autonomic nervous system work by mimicking or altering the functions of acetylcholine and norepinephrine in the cholinergic and adrenergic neurons of the sympathetic and parasympathetic systems. The document outlines the locations and mechanisms of action of muscarinic, nicotinic, alpha, beta, and dopamine receptors that are targeted by cholinergic and adrenergic drugs.