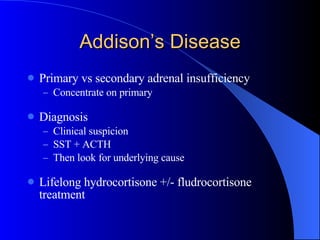
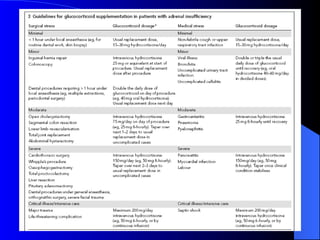
- Addison's disease is a condition where the adrenal glands do not produce enough hormones like cortisol. It requires lifelong treatment with hydrocortisone and sometimes fludrocortisone.
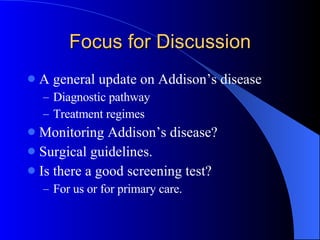
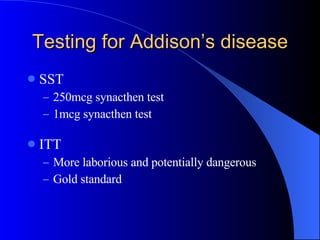
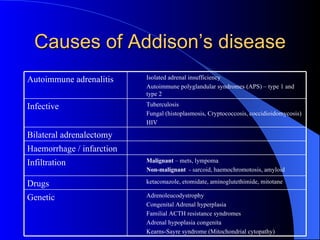
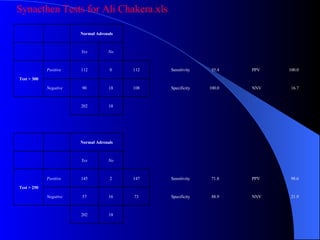
- The document discusses diagnostic testing for Addison's disease including the short synacthen test, causes of the condition, and monitoring and treatment options. It also presents results from synacthen tests at the author's hospital over the past few years.
- Based on the results, a baseline cortisol level greater than 350 nmol/L reliably ruled out adrenal insufficiency in patients, suggesting it could be a useful screening test for primary care physicians.