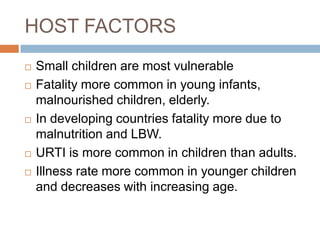
1. Acute respiratory illness (ARI) is a major cause of mortality and morbidity worldwide, especially in young children under 5 years old. Pneumonia accounts for 90% of ARI deaths and is commonly caused by bacteria.
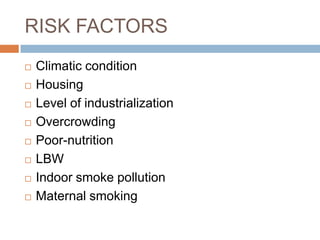
2. Developing countries have high rates of ARI due to factors like malnutrition, indoor smoke pollution, and overcrowding. Bangladesh, India, Indonesia and Nepal account for 40% of global ARI mortality.
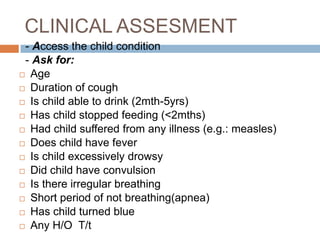
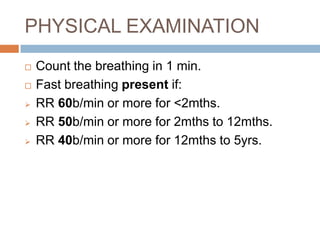
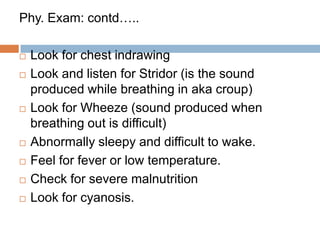
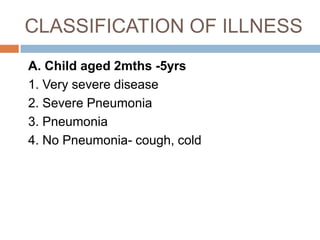
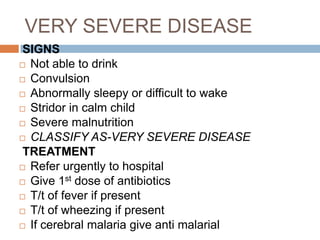
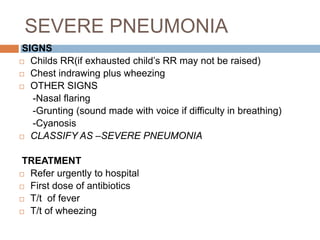
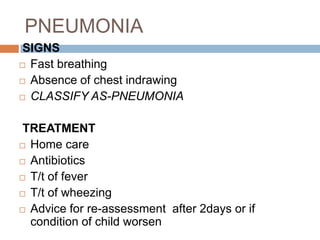
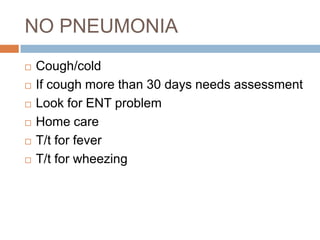
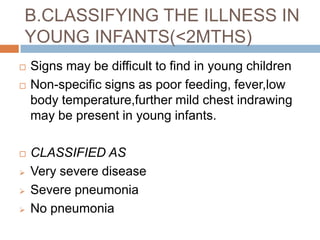
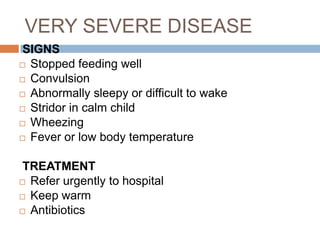
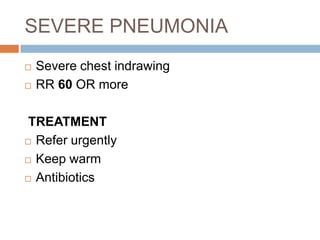
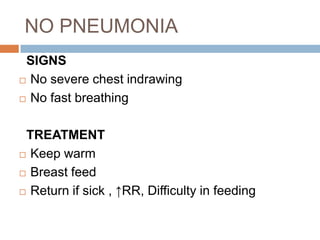
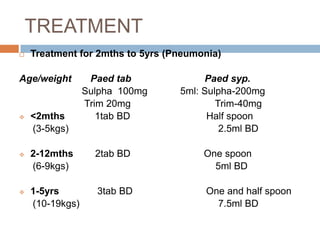
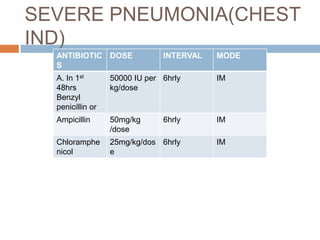
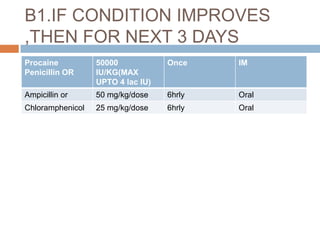
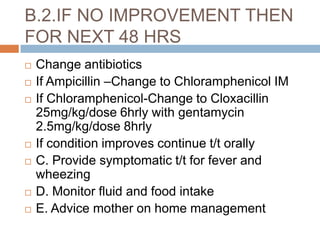
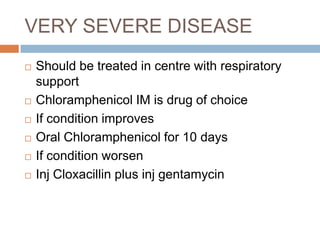
3. Clinical assessment of children with suspected ARI involves checking for symptoms like fast breathing and chest indrawing. Illnesses are classified as very severe, severe pneumonia, pneumonia, or no pneumonia to determine appropriate treatment.