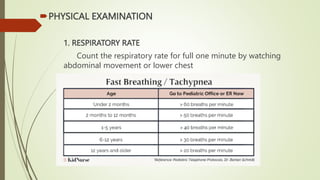
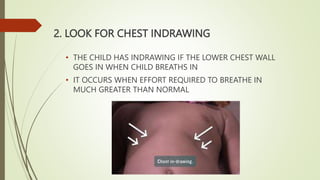
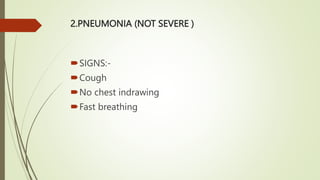
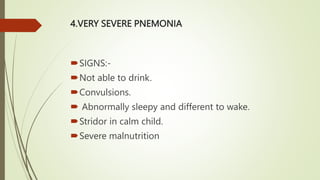
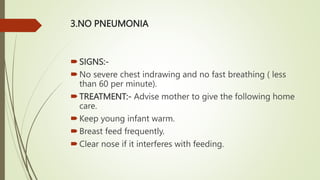
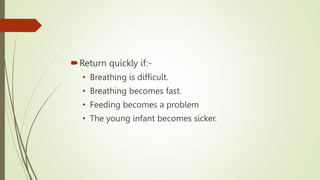
The document outlines acute respiratory infection (ARI) control measures, focusing on the classification, diagnosis, and treatment of ARIs in children, especially pneumonia. It details the signs of severity ranging from no pneumonia to very severe pneumonia, along with appropriate treatment protocols including referral to hospitals and antibiotic use. Additionally, it emphasizes preventive measures such as breastfeeding, immunization, and proper nutrition to reduce ARI incidence.