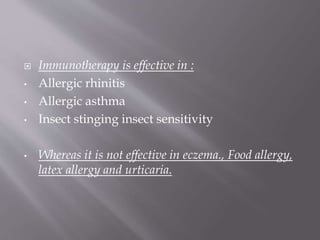
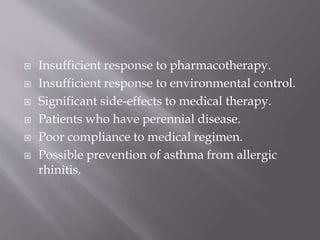
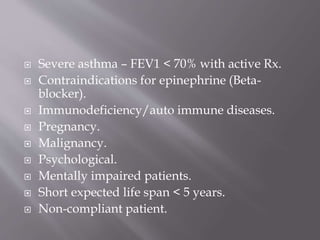
Allergen-specific immunotherapy involves administering increasing doses of allergens to induce tolerance. It works by inducing regulatory T cells that reduce the allergic response. Immunotherapy is effective for allergic rhinitis, asthma, and insect sensitivity. The goals are to eliminate symptoms or reduce medication needs. It is a safe and effective therapy when administered properly to suitable candidates.