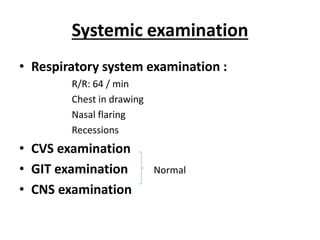
This document discusses acute respiratory tract infections in children. It provides details on a case of a 15 month old boy presenting with rhinorrhea, cough, fever and breathing difficulty. It discusses the classification, signs, and management of acute respiratory tract infections according to the WHO IMNCI protocol. The key points are: acute respiratory infections are a leading cause of death in children under 5 worldwide. Clinical assessment involves checking breathing rate, chest indrawing, fever and other danger signs. Conditions are classified as no pneumonia, pneumonia, severe pneumonia or very severe disease depending on symptoms. Management ranges from home care to hospitalization and antibiotics depending on severity of illness.